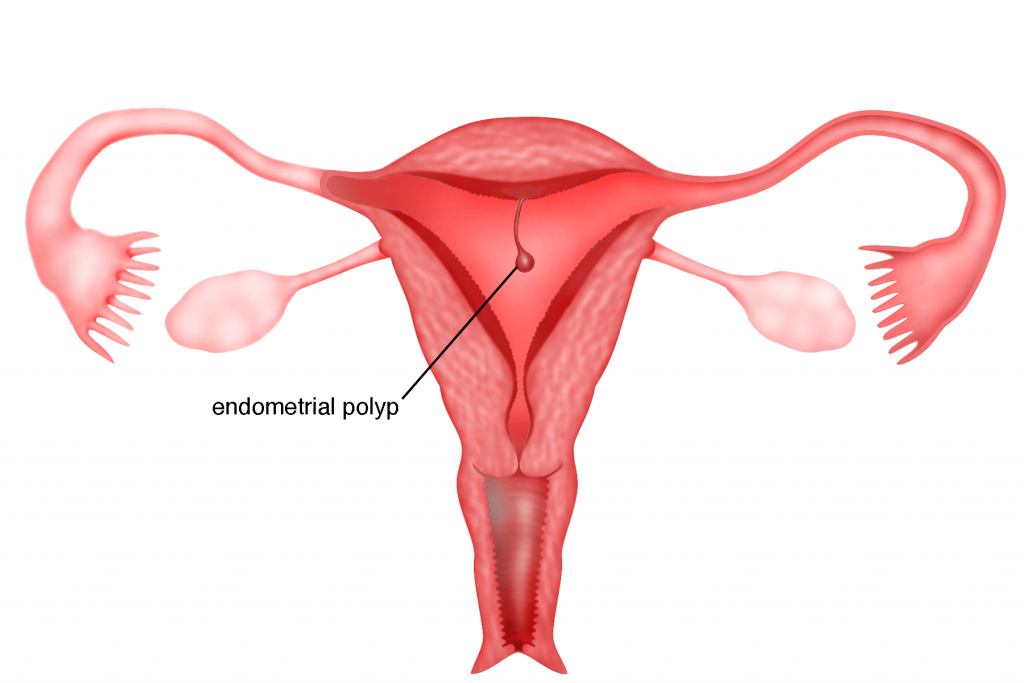
Endometrial polyps also known as uterine polyps, are outgrowths of the inner lining of the uterus (endometrium) protruding into the endometrial cavity. They may be attached to the endometrial cavity by a thin stalk (pedunculated polyps) or a broad base (sessile polyps). Pedunculated polyps are more common than sessile polyps. Their sizes range from a few millimetres to a few centimetres. There may be one or several polyps. Sometimes a pedunculated polyp can protrude through the cervix and into the vagina. Small blood vessels may be found especially on large polyps. Endometrial polyps are usually benign (non- cancerous) but sometimes they can turn malignant (cancer).
Causes
The cause of the formation of a polyp is unknown. The endometrium is under the influence of the hormone oestrogen and excessive oestrogen may cause the development of polyps.
Risk factors
Endometrial polyps are more common in women in their 40’s and 50’s. These polyps can form in postmenopausal women but rarely in women younger than 20 years of age. It is also more common in women who are overweight or obese with high blood pressure. Women who are on tamoxifen (a drug used to treat breast cancer) and on Hormone Replacement Therapy are also at increased risk of developing endometrial polyps.
Symptoms
Endometrial polyps can be asymptomatic and only detected during a routine ultrasound examination. Other symptoms are:
1) Bleeding or spotting in between periods
(intermenstrual bleeding)
2) Bleeding after sexual intercourse
(post coital bleeding)
3) Heavy menses
4) Painful menses (dysmenorrhoea)
This may occur when the polyp protrudes through the cervix and into the vagina
5) Inability to conceive (infertility)
The presence of a polyp may be the cause of the inability to conceive. A polyp may prevent the implantation of an embryo. Sometimes a polyp may increase the risk of miscarriage.
6) Bleeding or spotting after menopause
Case 6.1 : Endometrial polyp that was a cancer
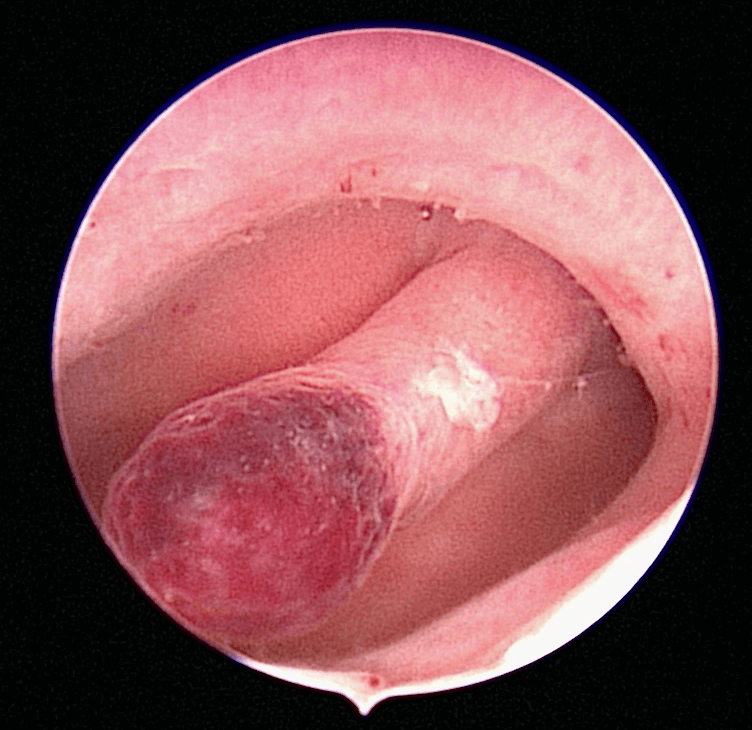
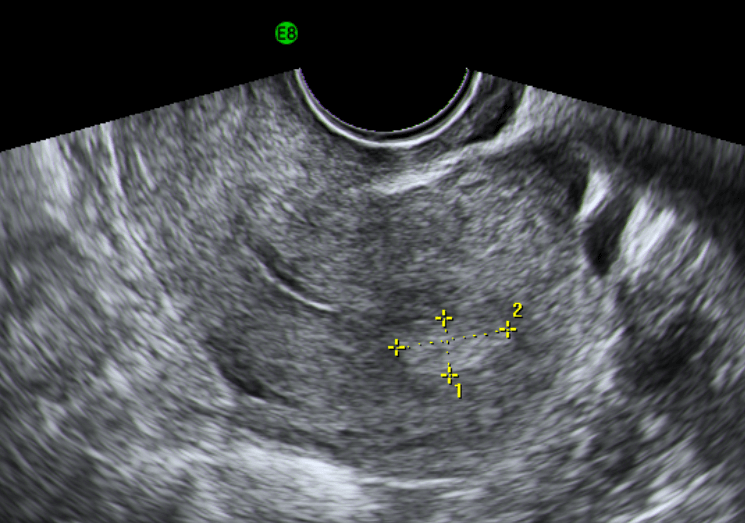
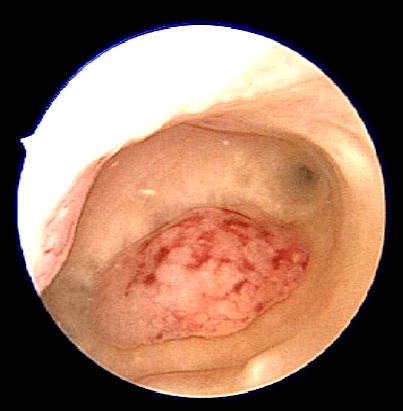
Madam LPH was a 52 year old lady who had her last normal menstrual periods on April 2013. She presented to me in October 2014 with a problem of postmenopausal per vaginal menstrual spotting. Transvaginal ultrasound done showed a bulky uterus with multiple small uterine fibroid, the biggest measuring 2.56 x 2.23 cm. There was a cystic endometrial polyp measuring about 1 cm (Figure 6.4). She underwent an office hysteroscopy and the polyp was removed (Figure 6.5). Histopathology showed that the polyp was hyperplastic with suspicion of adenocarcinoma. She underwent a total laparoscopic hysterectomy, bilateral salpingoopherectomy and pelvic lymph node sampling in November 2014. Histopathology of the uterus did not show any residual cancer of the endometrium.
Discussion
Bleeding after menopause requires investigation. This is especially so when the endometrium is thickened or if a polyp is seen in the endometrial cavity. In this patient the endometrial polyp removed was malignant but fortunately the endometrial cavity was not involved. Removal of the uterus cured her cancer.
Case 6.2 : Removal of an endometrial polyp in a subfertile lady leads to a natural pregnancy
Madam LSY saw me in November 2013 with a problem of inability to conceive. She had a child 7 years of age and was trying to conceive again the past 5 years. On examination and ultrasound, several small fibroids were seen in the uterus. The endometrial cavity was thickened. She underwent an office hysteroscopy and a large endometrial polyp was seen. The polyp was cut into 3 pieces and removed. She missed her periods in February 2014 and pregnancy test taken was positive. She delivered a healthy baby girl in October 2014.
Discussion
Endometrial polyp could be one of the cause of infertility. When the endometrium is thick, a hysteroscopy can assist in the diagnosis and removal of the polyp.
Diagnosis
Endometrial polyps can be suspected when a patient has the symptoms discussed above. Investigations will include:
1) Transvaginal Ultrasound
This is a procedure whereby an ultrasound probe is placed into the vagina to visualise the uterus and the endometrial cavity. Any irregularities in the endometrial cavity may indicate an endometrial polyp. However, in some women who have a thickened endometrial lining, a polyp may be missed.
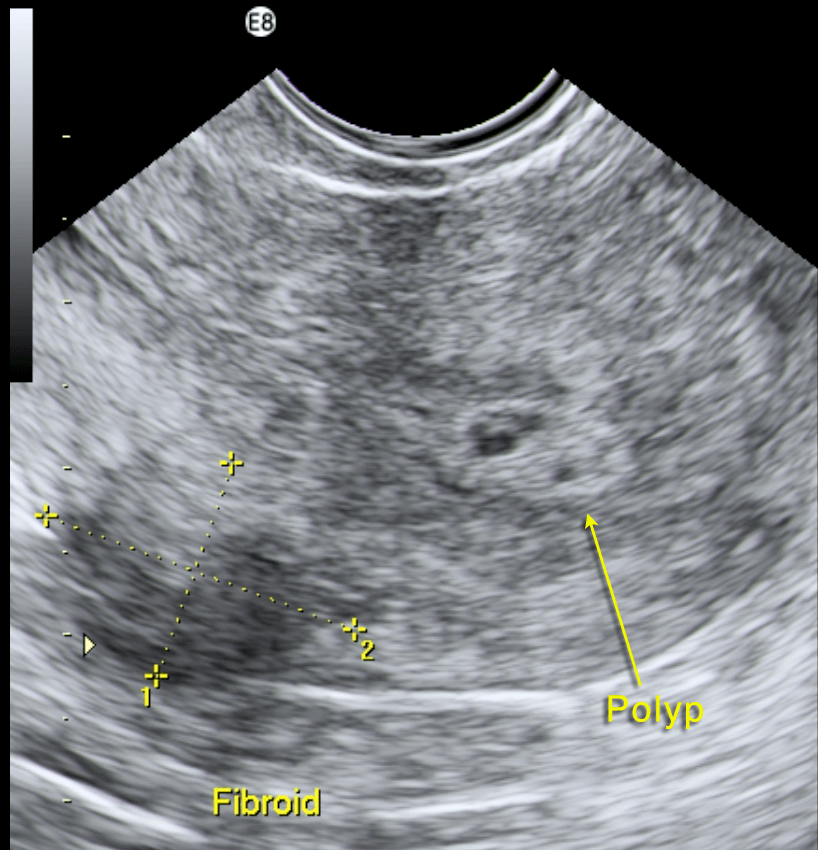
2) Sonohysterography
A thin tube is introduced into the uterine cavity and sterile fluid (saline – salt water) is injected to distend the cavity. A transvaginal or transabdominal ultrasound scan is performed at the same time. The presence of fluid in the endometrial cavity will be able to provide a clearer picture of any growth within the endometrial cavity (see Figure 41.6).
3) Hysteroscopy
This procedure is performed by placing a thin telescope (hysteroscope) through the cervix and into the uterine cavity via the vagina. It is usually done in the clinic without any anaesthesia. The hysteroscope is attached to a camera system and the endometrial cavity can be visualised on a monitor. Any polyp present can be seen and even removed simultaneously (see chapter 38).
Treatment
The following treatment may be recommended
1) Watchful waiting
Asymptomatic polyps may resolve on their own. A repeat ultrasound can be done after 3 to 6 months to see whether the polyp is still present.
2) Medication
Hormones such as progestin (g) may be given to shrink the polyps. Even if the polyp shrinks, it may reappear when the hormones are stopped.
3) Hysteroscopy and removal of the polyp
This minor surgery is usually performed under anaesthesia. A hysteroscopy is performed and the polyp can be excised using slender instruments such as graspers and scissors.
4) Curettage
A slender instrument is placed into the endometrial cavity and the inner lining of the uterus is scraped to remove all the polyps. This may be performed with the assistance
of a hysteroscope to ensue that all the polyps have been removed and the endometrial cavity is empty.
Postoperative Management
If the histopathology (g) reports states that the polyp is benign, then regular follow-up is necessary to ensure that it does
not recur. Rarely, do endometrial polyps recur. However, if the polyps are pre-cancerous or malignant (cancer) then further treatment will be necessary (see chapter 33)
Prevention
There is no way of preventing the occurrence of endometrial polyps. All women, especially those women with the risk factors mentioned above, will need regular gynaecological examination and transvaginal ultrasound scans.

Summary
Endometrial polyps, also known as uterine polyps, are outgrowths of the inner lining of the uterus (endometrium,) protruding into the endometrial cavity. They can vary in size and number. They usually present with intermenstrual bleeding. Diagnosis is made by transvaginal ultrasound, sonohysterography and hysteroscopy. Treatment includes watchful waiting, medication to shrink the polyps, hysteroscopic removal of the polyp or curettage.
