An Ovarian Cyst is a sac or pouch that develops in the ovary. The cyst may contain liquid, or solid material or a combination of both. The fluid within the cyst can range from thin and watery to thick and paste-like. The wall that covers the cyst can be thin or thick.
Ovarian cysts are very common, particularly in women between the ages of 30 and 60. They may be single or multiple and can occur in one or both ovaries. Most are benign (non-cancerous), but a small percentage can be malignant (cancerous).
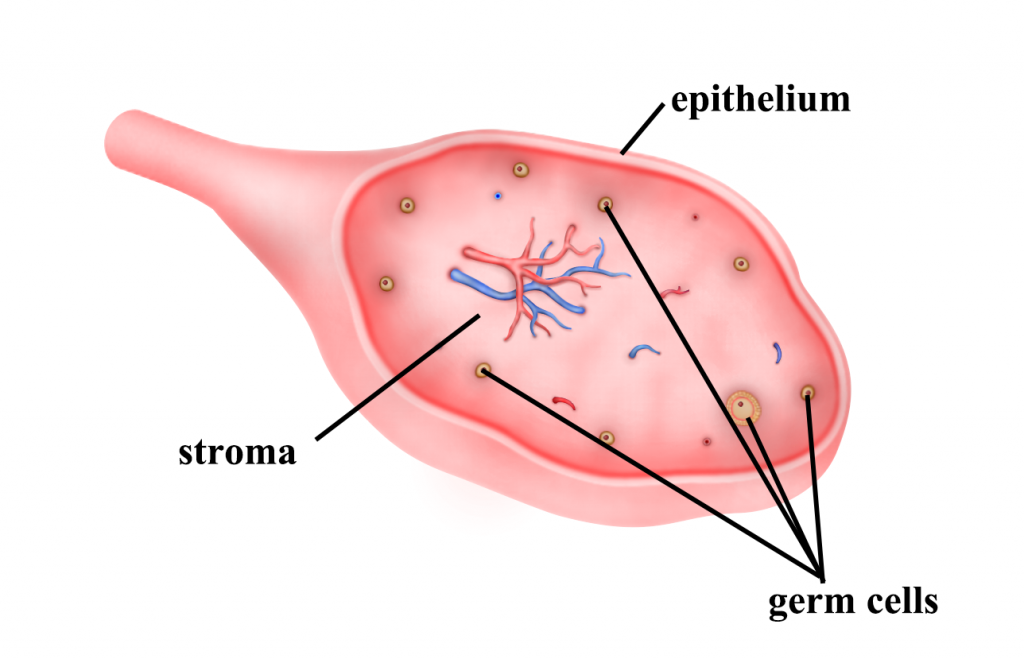
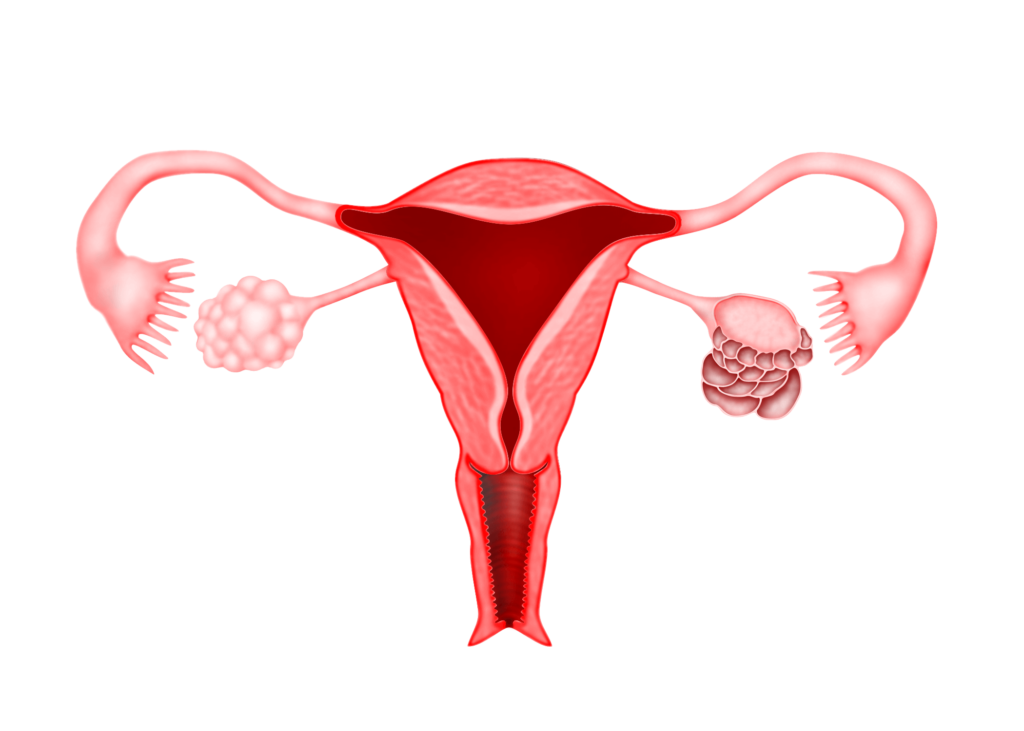
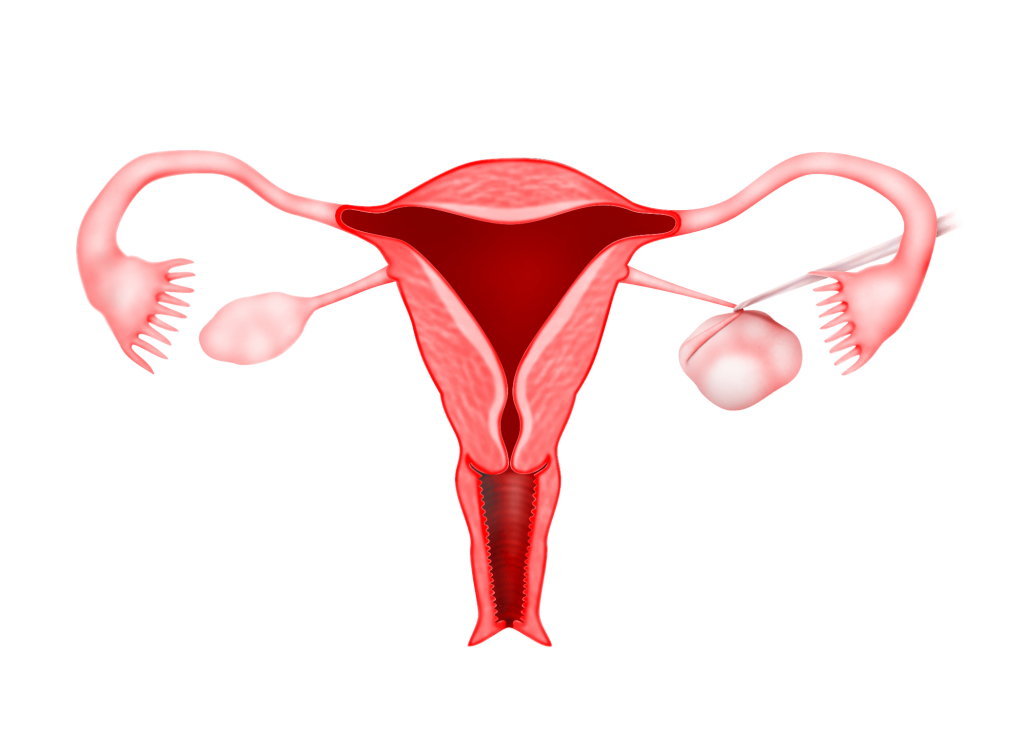
The Ovary
The ovary consists of several parts. The covering is call the epithelium, the central part is call the stroma and there are cells in the centre called the germ cells, which produce the eggs. Cysts can form from any part of the ovary.
Types of cysts
There are several different kinds of ovarian cysts, which are categorised as either:
1) Functional cysts (the most common type):
harmless cysts that form as part of the menstrual cycle, or
2) Pathological cysts:
tumours in the ovaries that are either benign (harmless) or malignant (cancerous).
Functional cysts
There are two types of functional ovarian cysts: the Follicular cyst and the Luteal cyst.
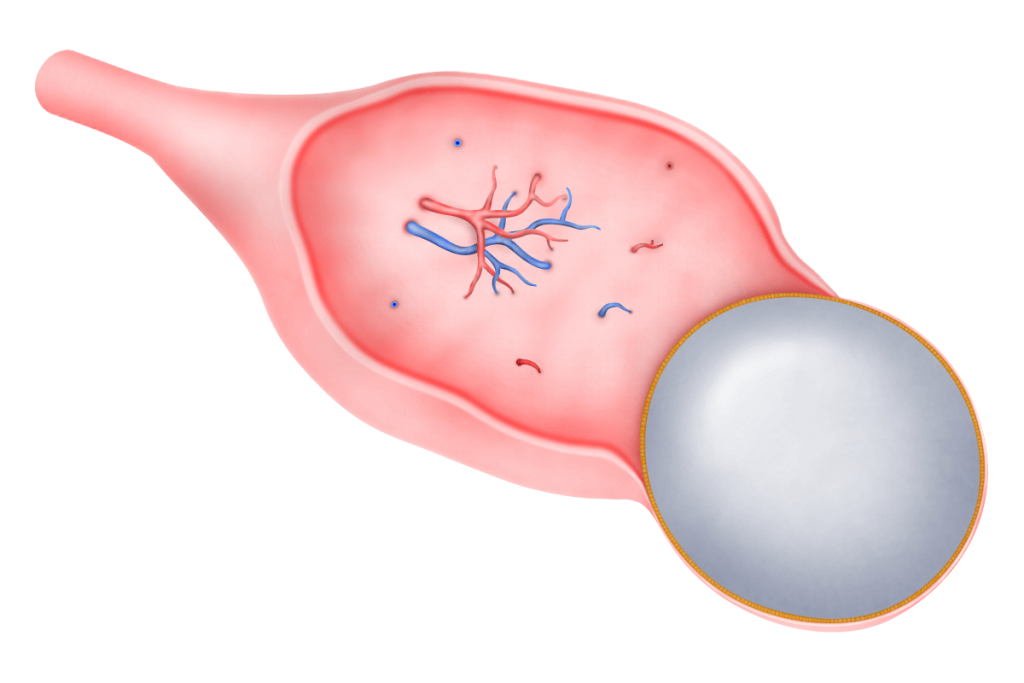
a) Follicular cysts
Follicular cysts are the most commonly seen ovarian cysts. During the early part of the menstrual cycle, a follicle develops in the ovary. The follicle contains fluid to protect the egg as it grows. During ovulation the follicle bursts and releases an egg. After that, it becomes a corpus luteum and shrinks. Sometimes, a follicle does not release an egg and does not shed its fluid. If this happens,
the follicle can get bigger as it swells with fluid. This becomes a follicular ovarian cyst. Usually, only one cyst appears at a time. Sometimes, however, more than 1 follicular cyst may be present if medication to induce ovulation (fertility drugs) are taken. It normally goes away without treatment after a few weeks.
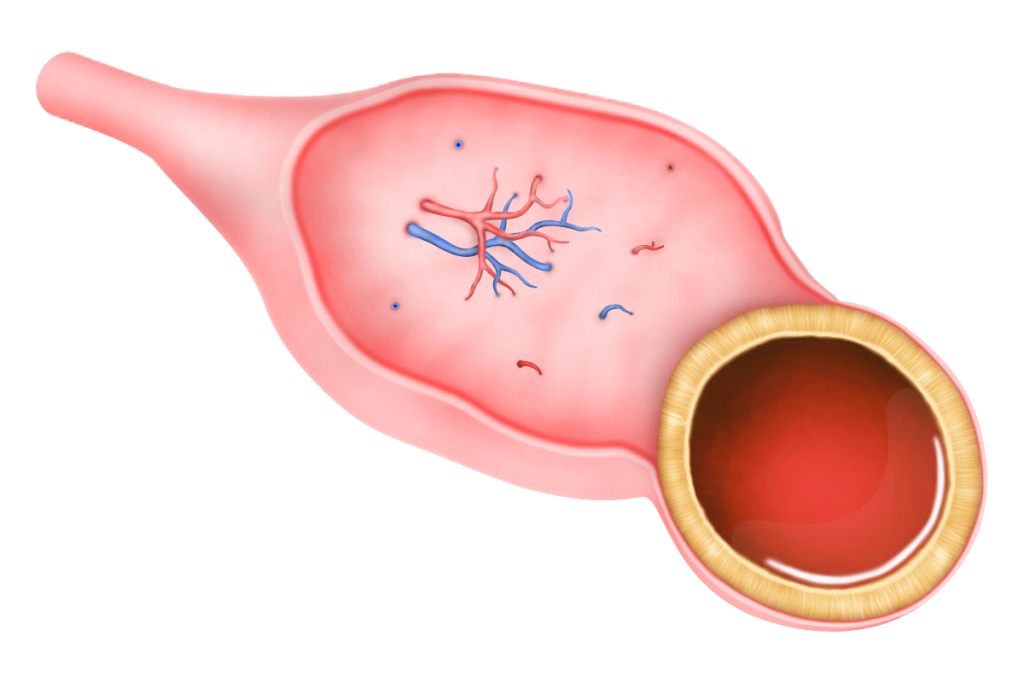
b) Luteal cysts
Luteal cysts are less common. They develop when the tissue that is left behind after an egg has been released (the corpus luteum), fills with blood. Luteal cysts usually disappear on their own within a few months, but can sometimes rupture, causing internal bleeding and sudden pain.
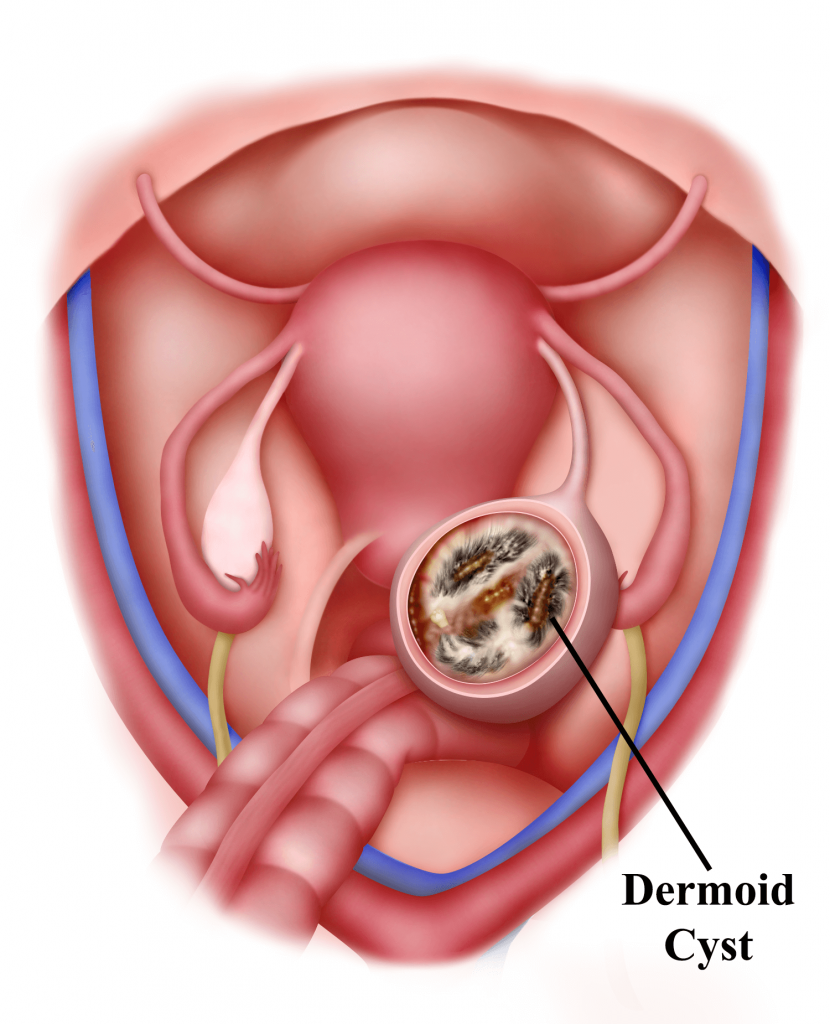
Pathological cysts
Cysts can develop from different parts of the ovary. The most common cysts that develop from the germ cells that form the eggs are the dermoid cysts. The most common cysts that develop from the epithelium (covering of the ovary) are called cystadenoma. Cysts can develop from the stromal layer as well but they are rare. In women under the age of 30, dermoid cysts are the most common type of pathological cysts. Past the age of 40, tumours called cystadenomas are the most common type of pathological cysts.
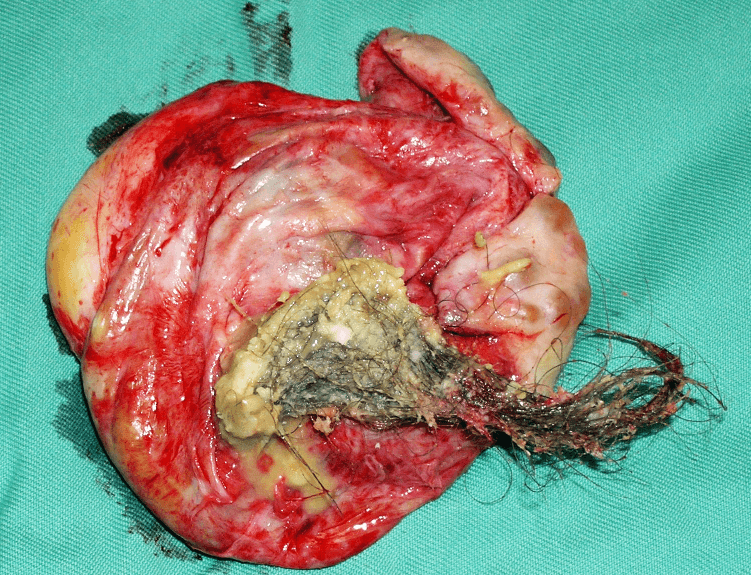
a) Dermoid cysts
(sometimes called benign mature cystic teratomas)
Dermoid cysts tend to occur in younger women. These cysts are present at birth but are not noticed until adulthood They can grow to be quite large – up to 15 cm across. Dermoid cysts often contain odd contents such as hair, parts of teeth or bone, fatty tissue, etc. This is because these cysts develop from the ovary’s germ cells, which make eggs in the ovary. These cells have the potential to develop into any type of cell and so can make different types of tissue. In about 1 in every 10 cases, a dermoid cyst develops in both ovaries. Dermoid cysts can be hereditary. They could occasionally become malignant (cancerous) and may need to be surgically removed. Dermoid cysts can be removed by laparoscopy (see Chapter 27).
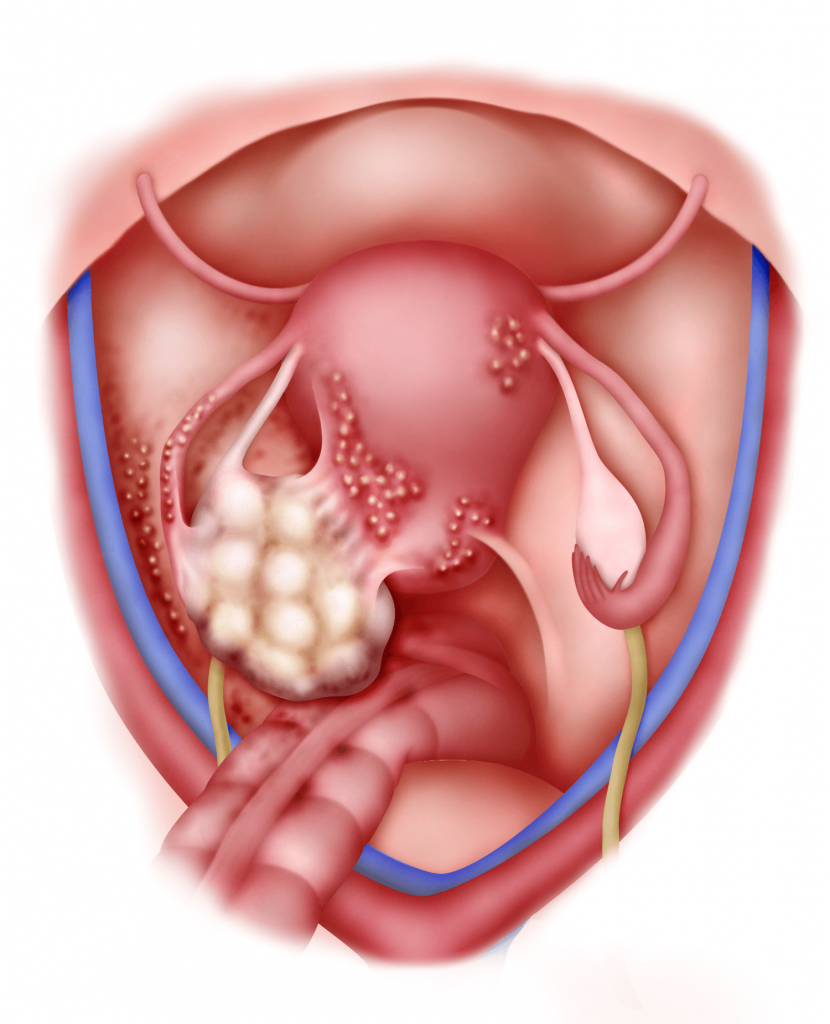
b) Cystadenomas
Cystadenomas develop from cells that cover the outer part of the ovary (epithelium). Cystadenomas are often attached to an ovary by a stalk rather than growing inside the ovary itself. This means that they can grow to a large size. They are not normally cancerous, but need to be surgically removed. There are two (2) types of cystadenomas – serous and mucinous. A serous cystadenoma is filled with a thin watery fluid. A mucinous cystadenoma is filled with a sticky, thick gelatinous material.
Conditions causing Cysts
1) Endometriosis
Patients with endometriosis may develop ovarian cysts called endometrioma or “chocolate cyst”. (see Chapters 3 and 25)
2) Polycystic Ovarian Syndrome
In this condition, many small, harmless cysts develop in the ovaries. The cysts develop because of an imbalance of hormones produced by the ovaries (see Chapter 23).
Symptoms
Most ovarian cysts are small, benign (harmless) and do not cause any symptoms. Large cysts may cause problems and the symptoms may be as follows:
1) Pain and discomfort in the abdomen
This may come and go, but it may last for long periods of time. Some women notice it more after sex.
2) Bloating or swelling in the abdomen.
3) Changes to Periods
They may become irregular, painful, heavier or lighter than normal.
4) Needing to visit the toilet more often
Depending on where the cyst is and its size, it may put pressure on the bladder or bowels. It may also cause pain during bowel movement.
5) Changes in the way breasts and body hair grow
In rare cases, ovarian cysts can cause abnormal amounts of hormones to be produced. These can speed up or change the way breasts and body hair grow.
Some medical conditions may cause additional symptoms:
1) Endometriosis may cause pelvic pain and lower back pain.
2) Polycystic Ovarian syndrome
(multiple cysts in the ovaries) may cause weight gain and acne.
Symptoms of complicated cysts
Sometimes, ovarian cysts can cause more serious problems. These are outlined below.
1) Torsion
If a cyst is growing on a stem from an ovary, the stem can become twisted. This is called torsion. Torsion stops blood supply to the cyst and causes a lot of pain in the lower abdomen.
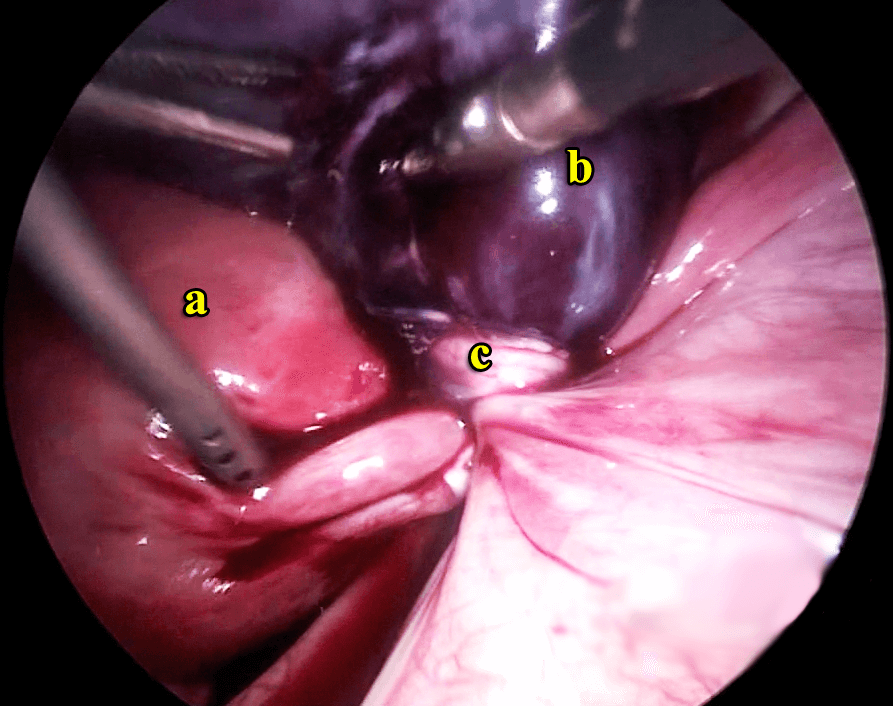

Twisted ovarian cyst laparoscopic right salpingoophrectomy
https://vimeo.com/149700129
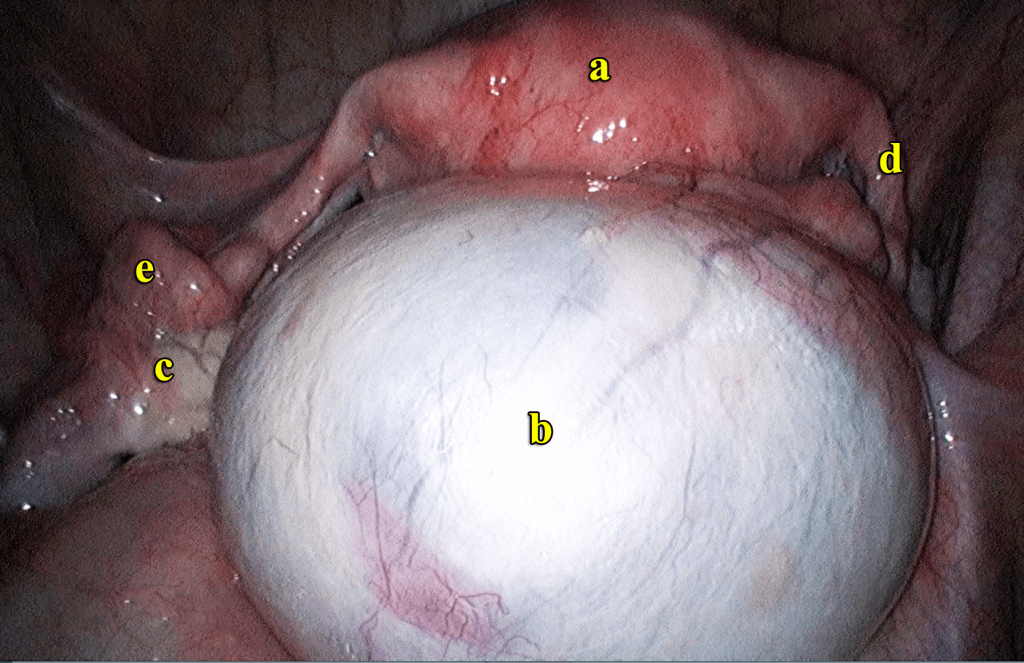
Case 5.1 : Twisted gangrenous ovarian cyst
ZH came to see me in November 2013 with a problem of lower abdominal pain. She had missed her periods for 3 months. Examination and ultrasound showed an intrauterine gestational sac with a fetus measuring 10 gestational weeks but with no foetal heart activity, indicating miscarriage. She also had 2 large right ovarian cysts with solid and cystic components in them. The cysts measured 5.55 x 6.98 and 4.28 x 3.81 cm. The patient felt pain on palpation of the cysts. Her tumour markers showed a raised serum CA 125 (97.6 mIU) , normal serum alpha feto protein (3.42mIU) and raised serum beta HCG (121550 miu/ml).
She underwent a suction curettage to remove the miscarriage. This was followed by a laparoscopy which showed a twisted ovarian cyst which was gangrenous. Laparoscopic right salpingectomy was performed. Postoperatively she has been well.
Discussion
Pelvic pain in a patient with an ovarian cyst is a surgical emergency. This is because if the twisted ovarian cyst is still not gangrenous, it can be untwisted. If the blood flow to the ovary is restored, the ovary can be saved by just removing the cyst (cystectomy). However, as in this case, if the cyst is gangrenous, the ovary has to be removed.
2) Bursting
The cyst may burst, causing sudden severe pain in the lower abdomen. The pain felt depends on what the cyst contains, whether it is infected and whether there is any bleeding.
3) Cancer
Occasionally, an ovarian cyst is an early form of ovarian cancer. However, ovarian cysts are very common and about 95% are non-cancerous.

Diagnosis of ovarian cyst
As most ovarian cysts cause no symptoms, many cysts are diagnosed by chance. It may be diagnosed during a routine examination or when an ultrasound is done for other reasons. If a patient has symptoms suggestive of an ovarian cyst, an abdominal and vaginal examination may be done. The doctor may feel an abnormal swelling which may be a cyst. Tests that may be done are as follows:
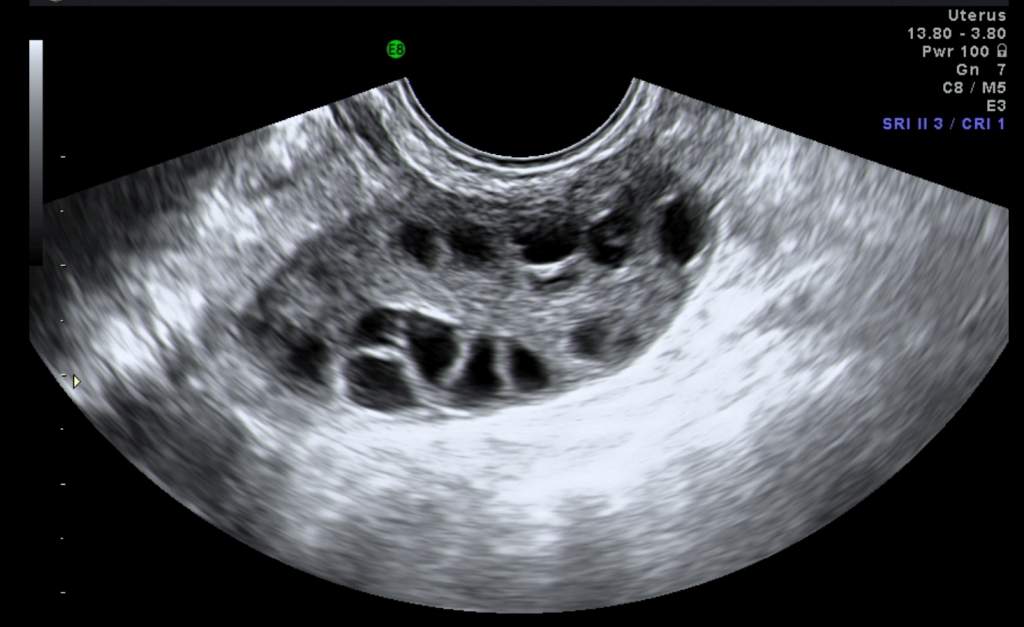
1) Ultrasound
An ultrasound scan can confirm an ovarian cyst. An ultrasound scan is safe and painless. It uses sound waves to create images of organs and structures inside the body. The probe of the scanner may be placed on the abdomen to scan the ovaries. A small probe is also often placed inside the vagina of the patient to scan the ovaries to obtain more detailed images. With an ultrasound, the doctor can see the cyst’s shape, size, location and its contents (fluid-filled, solid, or mixed).

2) A pregnancy test
This test may be done to rule out pregnancy.
3) Hormone level tests
Hormone levels may be checked to see if there are hormone-related problems.
4) A blood test
This test is done to find out if the cyst is cancerous. The test measures a substance in the blood called Cancer-Antigen 125 (CA-125). The amount of CA-125 is higher with ovarian cancer. Some ovarian cancers do not make enough CA- 125 to be detected by the test. Some noncancerous diseases such as endometriosis also have raised CA-125 levels. Noncancerous causes of higher CA-125 are more common in women younger than 35 years old. Ovarian cancer is very rare in this age group. The CA-125 test is most often done on women who are older than 35, as they are at high risk for ovarian cancer or have a cyst that is partly solid.
Treatment for Ovarian Cysts
Treatment will depend on factors such as age, menopausal status, the appearance and size of the cyst from the ultrasound scan and whether there are symptoms.
1) Observation
For functional cysts a “watch and wait” approach is taken. Functional cysts tend to dissolve over time and treatment is not needed. A repeat ultrasound may be done usually after two menstrual cycles to ensure that the cyst has disappeared. In some patients, if the cyst recurs, birth control pills may be prescribed. These pills reduce the hormones that promote the growth of cysts and prevent the formation of large cysts.
Operation
Removal of an ovarian cyst may be advised, especially if there are symptoms or if the cyst is large. Sometimes removal of the cyst may be necessary to ensure that it is not cancerous. Most cysts can be removed by laparoscopic surgery (‘keyhole’ surgery). Some cysts, especially if cancer is suspected, may require a laparotomy. The type of operation depends on factors such as the type of cyst, the age, complications encountered such as bleeding, rupturing and twisting of the cyst, and whether cancer is suspected or ruled out. In some cases, just the cyst is removed (cystectomy) and the ovarian tissue preserved. In other cases, the cyst, ovary and the fallopian tube are removed (salpingooopherectomy).
In a worse scenario, the cyst with the ovary, as well as, the other ovary and uterus are all removed (hysterectomy and bilateral salpingoopherectomy). All these surgeries can be performed either by laparoscopy or laparotomy (see chapters 27 and 33).
Summary
Ovarian cysts are common in women. There are many types of ovarian cysts. Most ovarian cysts are benign and uncomplicated. Surgery is indicated if cysts are persistent, become bigger or cause symptoms. Most ovarian cysts can be removed by laparoscopic surgery

