Endometriosis is a disease in which the endometrial tissue, or the lining of the uterus, grows outside the uterus to its surrounding areas and even to distant parts of the body. This displaced endometrial tissue is influenced by female hormonal changes and responds to them in a similar way like the inner lining of the uterus, such as thickening, breaking down and even bleeding during menses. The ongoing process causes inflammation (g) in the surrounding areas and the formation of scar tissue, which usually distorts the anatomy of the surrounding organs and interferes with their functions.
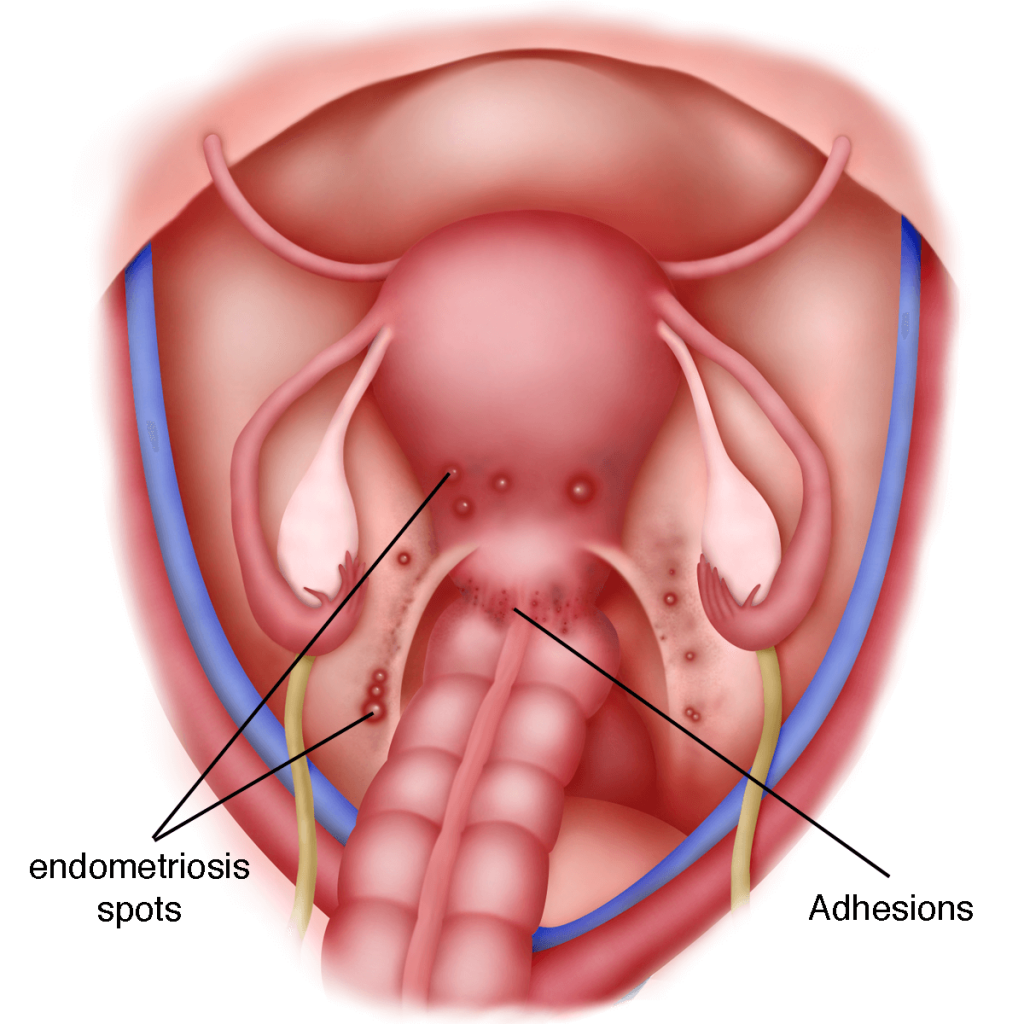
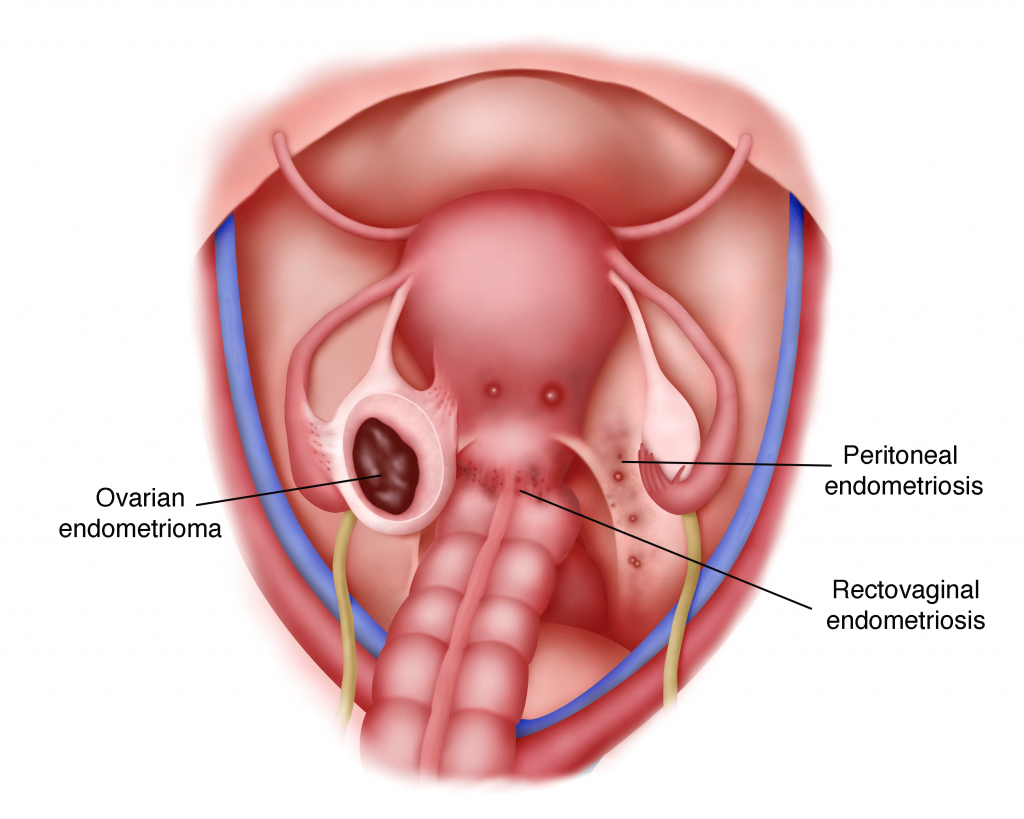
Endometriosis is highly prevalent and can be found anywhere in the body. The most common sites are the ovaries, the fallopian tubes, the pelvic sidewall, the uterosacral ligaments (g), the Pouch of Douglas (g) and the rectovaginal septum (g). Other less common sites are on the Caesarian section, laparoscopy or laparotomy scars, the bladder, bowel, intestines, colon, appendix, and rectum. In rare cases, endometriosis can invade the vagina, bladder, skin, lung, spine and even the brain.
Types of lesions
There are different types of lesions of endometriosis
1) Peritoneal endometriosis
Endometriotic lesions are seen on the peritoneal surface. It can be seen as many different lesions.
a) Black or bluish lesions
This is the most common type of lesion recognised at laparoscopy
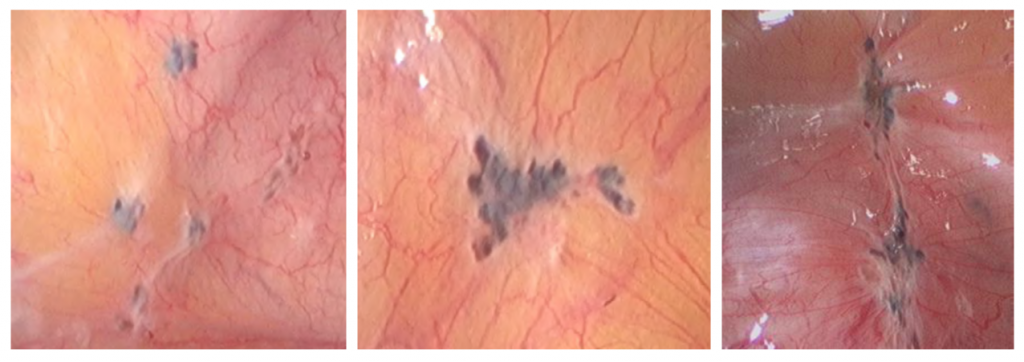
b) White lesions
White opacification of the peritoneum that looks like peritoneal scarring or patches. Some lesions will look yellowish brown while others appear as circular peritoneal defects.
c) Non-visible endometriosis
Some endometriotic lesions may not be seen in laparoscopy but only confirmed by biopsy
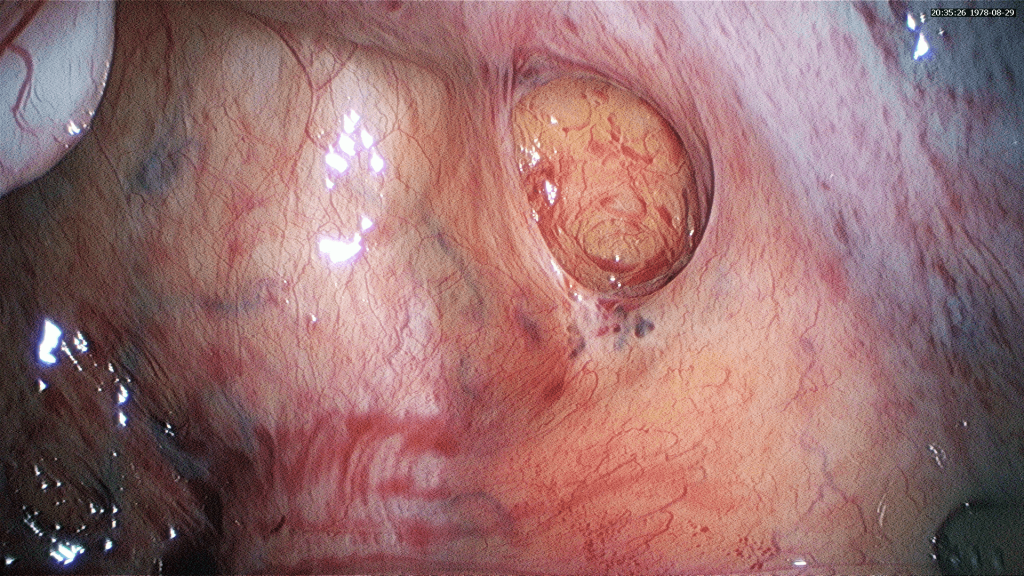
2. Ovarian Endometrioma
These are cysts seen in the ovaries. Their size may range from a few millimeters to several centimeters
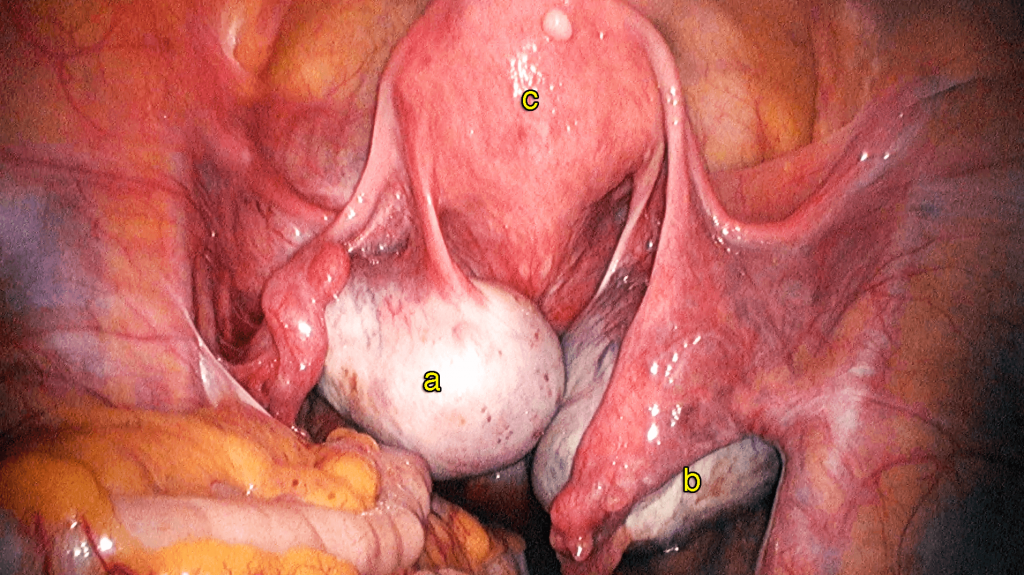
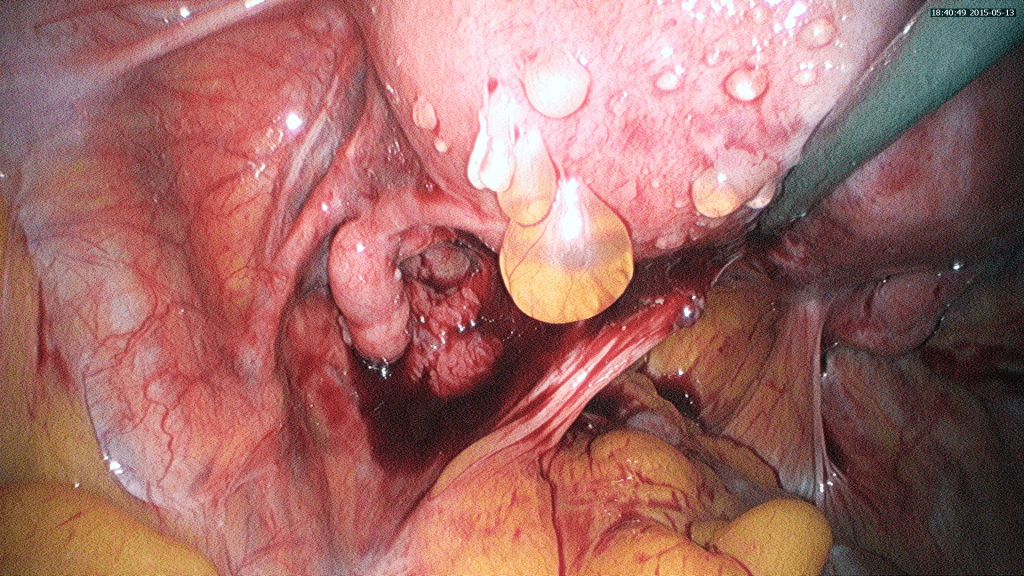
3. Rectovaginal Endometriosis
This type of endometriosis obliterates the Pouch of Douglas
Cause
There is no accurate explanation as to what causes endometriosis. Many theories have been formed to explain the origin of the disease. One of the most popular and widely believed theories is Sampson’s Theory of Retrograde Menstruation, postulated by Dr. John Sampson in the 1920’s. According to the theory, during menstruation each month, a certain amount of menstrual fluid (consisting of blood, endometrial tissue, etc.) in the uterus is forced backwards through the fallopian tube into the abdominal cavity. The body usually responds to this kind of spilling by reabsorbing the menstrual fluid back into the circulatory system. However, in some women, possibly due to an immune system dysfunction, the fluid (particularly the endometrial tissue) is not reabsorbed but instead implants itself and grows on the pelvic and abdominal organs as endometriosis.
Signs and Symptoms
1) Pelvic pain
Most women with endometriosis experience severe pelvic pain, lower back pain and cramps before and during menstruation. This is called dysmenorrhea. The pain is typically described
as aggravating as the menstruation progresses (e.g. the pain on day 4 of the menses is worse than that on day 1). Some women may also experience intense pain around the time of ovulation. There may be other signs that do not correlate with the menstrual cycle such as dyspareunia, (pain during intercourse), and dysuria (painful urination). For dysuria, blood may be occasionally seen in the urine.
2) Heavy or irregular vaginal bleeding
Women with endometriosis may experience excessive menstrual bleeding (menorrhagia) or bleeding between periods (menometrorrhagia).
3) Infertility
Some women with endometriosis may experience little or no pain at all but are unable to conceive and are usually first diagnosed with endometriosis while seeking treatment for infertility. These are usually cases where the formation of scar tissue (adhesions) due to endometriosis, has somehow distorted the reproductive organs and therefore results in inability to conceive.
4) Painful bowel movements
Some women may experience bowel pain followed by abdominal bloating, constipation, or diarrhoea. The pain may intensify during menstruation.
5) Rectal bleeding during menstruation.
Diagnosis
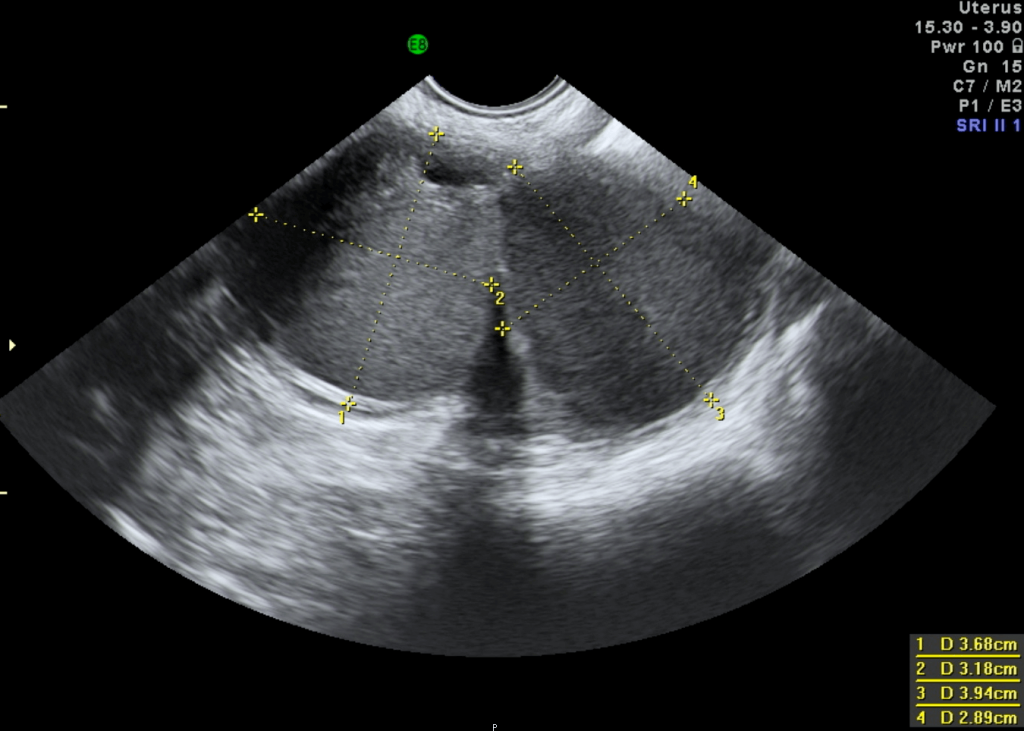
There are no specific tests to assess whether a woman has endometriosis. Exploring a patient’s medical history may give the doctor some clue to the presence of this disease, and it is usually corroborated by a pelvic examination. The pelvic examination may reveal nodularity in the Pouch of Douglas; uterine enlargement or irregularity: pelvic masses or pelvic tenderness. In cases of ovarian endometrioma (chocolate cyst), the ultrasound can detect ovarian cysts that appear in the form of black bubbles. Sometimes, the doctor may order a CA-125 test for the patient as it has been suggested that women with endometriosis are likely to have an elevated level of CA-125 (a cancer antigen) in their blood (see chapter 14). In any case, it is possible for endometriosis to be mistaken for other gynecological conditions that have similar symptoms and vice versa. The only reliable way to confirm and verify the suspected diagnosis of endometriosis is through laparoscopy.
Treatment Options
Due to the fact that the exact cause of endometriosis remains unknown, there is currently no absolute cure for this disease. There are, however, several treatment options that aim to relieve the pain of endometriosis and reduce its growth.
They are:
a) Pain medication
b) Surgery
c) Hormone therapy
a) Pain medication
Some women may experience pain for a short duration. For these patients, painkillers may be sufficient to relieve their symptoms. The types of painkillers administered range from simple analgesics such as paracetamol and aspirin, as well as nonsteriodal anti- inflammatory drugs (NSAIDS) for example Ponstan® and Syn- Flex®; to narcotic analgesic (drugs that are similar to morphine).
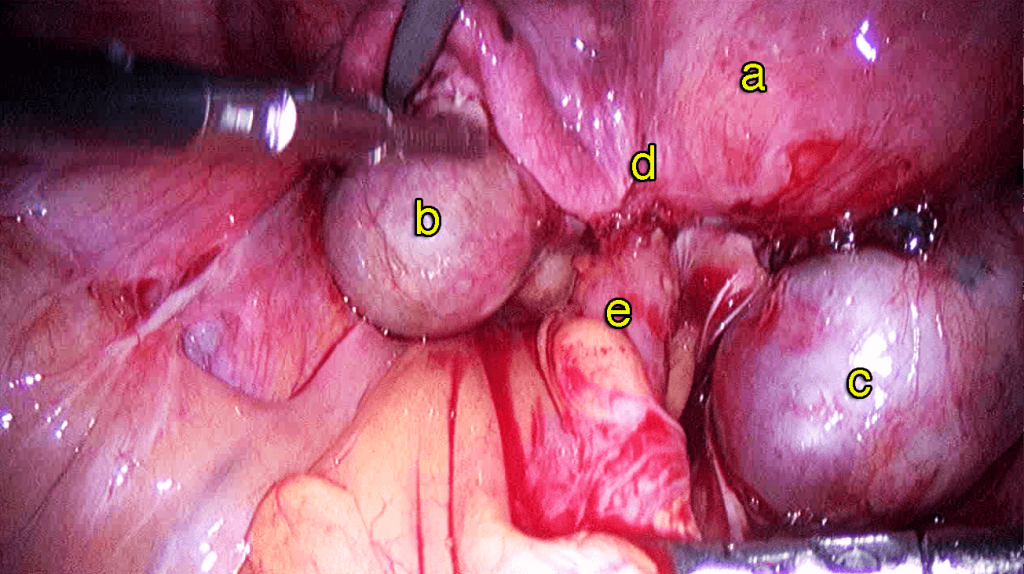
b) Surgery
Surgery is the main treatment option for women with endometriosis. Laparoscopic surgery can be performed to diagnose as well as, treat endometriosis at the same time. The aim of surgery is to diagnose the endometriosis as well as remove as much of the diseased areas as possible.
It is important to do all the necessary investigations to determine the severity of the disease prior to the surgery. The patient
should discuss with her gynaecologist the extent of surgery that needs to be performed. One must understand that the more extensive the surgery, the greater the risk of complications. Success of the surgery depends on the skill of the surgeon. An experienced laparoscopic surgeon will be able to excise all the endometriotic lesions in a single surgery. On rare occasions, a laparotomy may be necessary to excise extensive endometriosis.
c) Hormone therapy
Endometriosis is known to be exacerbated by the hormone oestrogen. Oestrogen is produced by the growing oocytes in the ovaries. Whenever there is menstruation the endometriotic lesion will also bleed, causing pain and the formation of adhesions.
Therefore, one way to suppress endometriosis growth and relieve its symptoms, is to lower oestrogen levels by preventing menstruation.
Hormonal therapies are usually given after laparoscopic surgery. Some of the therapies available are:
Gonadotropin-releasing hormone (GnRH) agonist
Combined oral contraceptive pills
Progestogens
Danazol
Dimetriose
Mirena® coil
Aromatase inhibitors
Case 3.1 : Spontaneous pregnancy immediately after laparoscopic cystectomy for an endometrioma
SSP, a 29 year old lady who had been married for 1 year, came to see me in June 2014 for her inability to conceive. She was asymptomatic. Examination and ultrasound showed 2 right clear cysts measuring 4.22 x 6.66 cm and 3.09 x 3.76 cm and there were 2 left endometriomas measuring 2.05 x 1.89 cm and 1.75 x 2.25 cm. She underwent a laparoscopic cystectomy. Postoperatively, she was well. She was encouraged to conceive without any delay. She missed her menses in December and conceived spontaneously.
Discussion
Endometriosis and endometrioma cause infertility. Laparoscopic surgical removal of endometriosis and endometrioma, if performed well, can result in spontaneous pregnancy.

Laparoscopic cystectomy for endometrioma and ovarian cysts
http://vimeo.com/149998620
i) Gonadotrophin – Releasing hormone (GnRH) agonist Ovulation is controlled by 2 hormones that are produced by the pituitary gland.
The pituitary gland is located in the brain. Above the pituitary gland is the hypothalamus. The hypothalamus produces a hormone called the Gonadotrophin Releasing Hormone
which stimulates the pituitary gland to produce FSH and LH. The FSH and LH stimulate the oocytes or eggs in the ovaries to grow and the developing oocytes will produce oestrogen. Gonadotrophin Releasing Hormone agonist will block the stimulation of the pituitary gland by the gonadotrophin releasing hormone. This will cause the pituitary gland to stop producing any FSH and LH thus preventing the growth of the oocytes in the ovaries. As no oocytes are growing, oestrogen production will cease. The patient will stop menstruating. She will be in a menopausal state called pseudomenopause. GnRH agonist are given in either monthly or 3 monthly injections.
Disadvantage of GnRH agonist
The side effects of GnRH agonist are:
a) Menopausal symptoms such as hot flushes, sweating, dry vagina, mood swings
b) Osteoporosis – Thinning of the bones called osteoporosis can occur especially if the injections are given for a duration exceeding 9 months.
c) These injections are also expensive.
Advantages of GnRH analogues
GnRH agonist is an effective treatment in all women. Menstruation will cease. Since it is a monthly or 3 monthly injection there is also no need to remember to take tablets everyday.
ii) Oral Contraceptive pills (OCP)
The oral contraceptive (OCP) pill contains low doses of oestrogen and progesterone. It works by preventing ovulation and so prevents the ovaries from producing oestrogen. Each pack of oral contraceptive pills contain 21 tablets of active pills. Oral contraceptive pills are usually taken for 3 weeks with a 1 week break to induce menstruation. However 3 packs can be taken continuously for 9 weeks followed by a 1-week break. In this way the number of menstruation cycles in a year can be reduced from 12 to 4.
Oral contraceptive pills may be prescribed immediately after a laparoscopic surgery or after GnRH agonist treatment. Since oral contraceptive pills are cheap and with minimal side effects, they can be taken for many years until the patient is ready to conceive.
The advantages of OCP’s
The advantages of OCP’s are that they are cheap with less side effects and can be taken for a long duration of time.
The disadvantages of OCP’s
A tablet has to be taken everyday and it may cause irregular breakthrough bleeding while being taken everyday.
Case 3.2 : Successful spontaneous pregnancy after taking Oral Contraceptive Pills to decrease the recurrence rate of endometrioma
GRR saw me in July 2009 for a problem of dysmenorrhea. She was 36 years old and was still single. Examination and ultrasound showed a fibroid measuring 4.48 x 5.91cm on the fundus of the uterus and a left ovarian cyst resembling endometrioma measuring 5.72 x 4.29 cm. She underwent a laparoscopic cystectomy and myomectomy in October 2009. Postoperatively, she received 3, monthly doses of GnRH agonist injections. She was on regular follow up after that and in December 2010, a small uterine fibroid measuring 1.85 x 1.84 cm was noted. She was advised to take oral contraceptive pills (OCPs) continuously for 3 months with a 1-week break. She took the OCPs continuously (3 months continuously with a 1 week break in between) until she got married in March 2014. The fibroid re- mained small and there was no recurrence of endometrioma. She spontaneously conceived in November 2014 at the age of 41 yrs.
Discussion
Patients who have endometriosis and are not keen to conceive should receive treatment to prevent the recurrence of the disease. The cheapest and most convenient mode of treatment is Oral Contraceptive Pills taken continuously. This will decrease the number of menses in a year. As endometriosis is dependent on menstrual bleeding, less bleeding during menstruation will reduce the chances of recurrence of the disease.
iii) Progestogens
Progestogens are synthetic progesterone. They are given to prevent ovulation. Progestogens are usually given continuously. There are many types of progestogens available in the market.
An injectable progestogen available in the market is Depoprovera® (medroxy-progesterone acetate). This is a 3 monthly injection that prevents ovulation. The advantage of Depoprovera® is that it is a 3 monthly injection and the patient need not remember taking tablets. The disadvantage is that it causes intermittent bleeding. It may not be suitable for women intending to conceive in the future because
it takes a long time for a women to start ovulating after cessation of the injection. It can also lead to osteoporosis.
The newest oral progestagen in the market is dienogest called Visanne®. One of the side effects of oral progestogen such as dienogest is that it can cause irregular per vaginal bleeding. It is usually recommended for 6 to 9 months. Due to the absence of oestrogen, continuous progesterone therapy may lead to osteroporosis.
iv) Danazol and Gestrinone
Danazol and Gestrinone suppress endometriosis by making oestrogen levels lower and androgens (testosterone) (g) levels higher. They were commonly used in the 1980’s but are rarely used now. Danazol is usually given in high doses of 600 to 800mg a day for 6 to 12 months. Gestrinone is given at doses of 2.5 to 5mg twice a week for the same duration.
The side effects of danazol are:
Due to high androgen levels the side effects are namely weight gain, bigger muscles, oily skin, increased body hair and cramps.
Due to low oestrogen levels the side effects are namely low libido, hot flushes and smaller breasts.
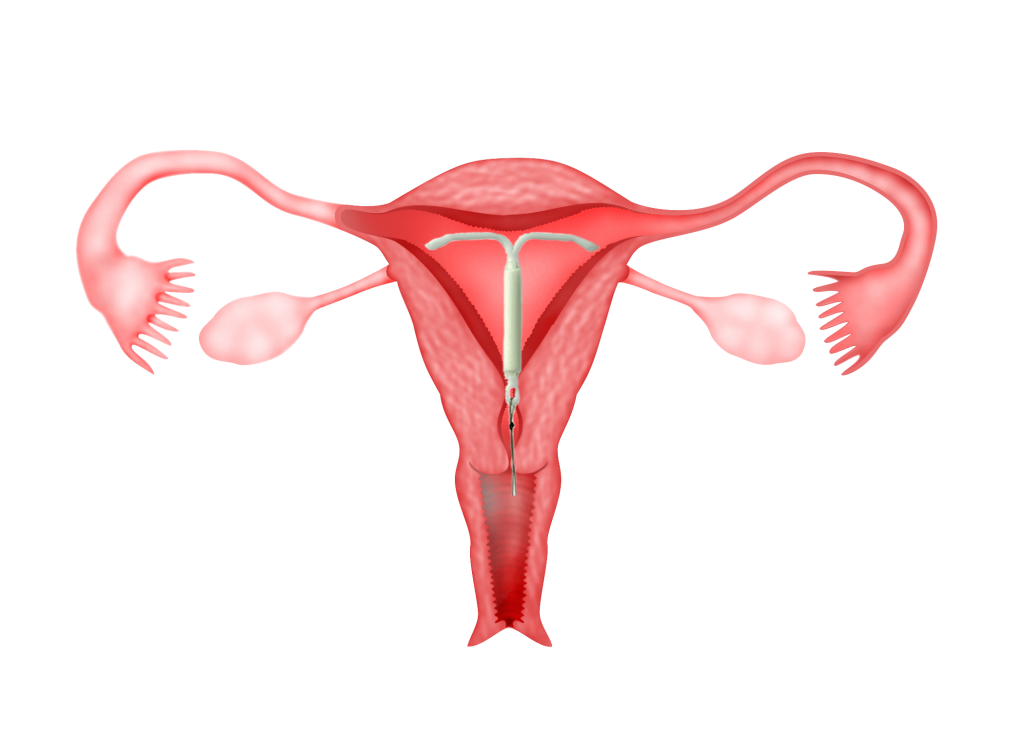
v) Mirena®
Mirena® is an intrauterine contraceptive device (IUCD) that contains a progesterone called levonogestrel. The uterus will absorb the progesterone causing a decrease in menstrual blood flow. When there is less menstrual blood flow, bleeding from the endometriosis will also decrease thus, suppressing the growth of the endometriosis. The Mirena can be left in the uterus for 5 years. The advantage of Mirena® is that the patient need not take daily medication. The amount of progesterone required to suppress menstruation is also very low because it is directly absorbed into the uterus. As only a small amount of progesterone reaches the rest of the body, the side effects of progesterone is minimal. The disadvantage of Mirena is that it may cause annoying irregular and prolonged spotting in some women. It is also not suitable for women who have not had sexual intercourse.
vi) Aromatase inhibitors
Aromatase is the hormone that converts testosterone to oestrogen. Aromatase inhibitors such as anastrozole and letrozole are drugs which inhibit the hormone aromatase. This will lead to a decrease in oestrogen production especially in the endometriotic lesions. The side effect of this medication is that it may lead to osteoporosis or bone thinning, tiredness and menopausal symptoms.
The choice of treatment for endometriosis depends on the patient’s age and individual needs, such as the desire to conceive and the severity of the symptoms. Some doctors prescribe hormonal treatment just based on the suspicion of endometriosis by history, examination and ultrasound. This is not recommended because most of the treatments have side effects and it is better to perform a laparoscopic surgery to confirm the disease before commencing medical treatment.
Can endometriosis recur after surgery?
Endometriosis can recur after surgery and medical treatment. The chances of recurrence are higher if an inexperienced surgeon performs the surgery and if most of the endometriotic lesions are not excised. If the patient is not contemplating pregnancy immediately after the surgery, continuing medical therapy is essential to suppress any endometriotic lesion that has not been excised. The cheapest treatment is Oral Contraceptive Pills.
Fact 3.1
Use of oral contraceptive pills in young unmarried women
Many young unmarried girls/women and their parents are worried when oral contraceptive pills (OCPs) are prescribed for endometriosis. Many have this fear that taking OCPs will lead to the inability to conceive in the future. This concept is wrong. The aim of prescribing OCPs in women who have undergone laparoscopic surgery for endometriosis, is to reduce the chances of a recurrence of the endometriosis. Endometriosis leads to infertility and by preventing its recurrence; OCPs actually increase the chances of pregnancy in the future
Summary
Endometriosis is a common gynaecological problem
It usually presents with pelvic pain especially during menses and during sexual intercourse. It also causes infertility
It can be suspected by taking a good medical history, performing a pelvic examination and a pelvic ultrasound scan.
Laparoscopy is the gold standard for the diagnosis and treatment of endometriosis.
Laparoscopic surgery for endometriosis can be difficult because endometriosis frequently involves vital structures such as the bowel, bladder and ureter. It is important for laparoscopic surgery to be performed by an experienced laparoscopic surgeon.
There are many medical treatments that can be prescribed after laparoscopic surgery to prevent the recurrence of the disease.

