Laparoscopy is considered the “gold standard” in diagnosing as well as treating endometriosis. Often, diagnosis and treatment are performed during the same operation. The surgical complexity can vary from as minor as destroying the endometriotic implants superficially with intense heat, to as major as removing and repairing the pelvic organs. As the disease usually affects these vital structures such as the bowel, ureters, bladder, blood vessels, etc., it is important to find a well-trained laparoscopic surgeon to treat the disease so that the risks can be kept minimal.
Types of Operations
The type of operation depends on the severity of the endometriosis. The more severe the condition, the more complex the operation, and the higher the risk it will pose. It is necessary for the patient to discuss thoroughly with her gynaecologist in order to understand the extent of the operation to be performed (prior to the surgery).
The following are the many types of operations available today:
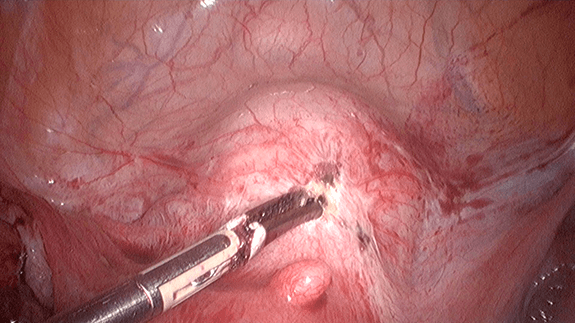
1) Coagulation
This procedure makes use of electric current or laser to “dry up” the endometriotic spots or nodules. It is relatively quick and easy, but it is difficult to ensure that the entire lesion has been thoroughly destroyed and will not regrow. In cases where vital structures are involved, the procedure must be done with extra care so that underlying normal tissues will not be damaged.
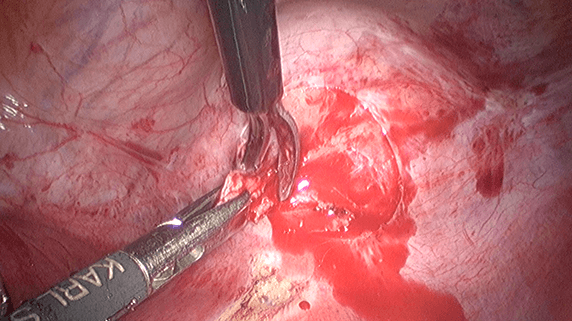
2) Excision of endometriotic implants
Excision is a better technique compared to coagulation but it requires special skills and experience. The surgeon must be familiar with the normal pelvic anatomy so that he will be able to excise all abnormal endometriotic implants. In cases where the vital organs are infiltrated by the lesion, the surgeon must be able to excise the lesion while keeping the organs as normal as possible.
If a vital organ has to be partially excised, the surgeon must be able to repair it so that its function will not be compromised.
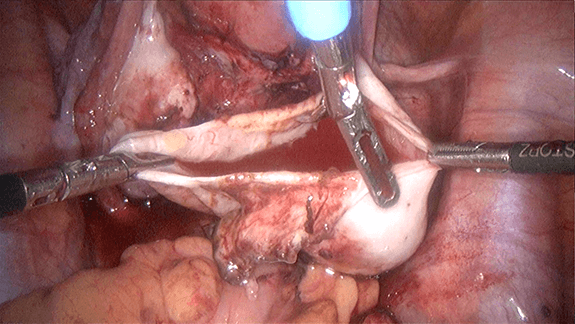
3) Excision of endometriotic cyst wall (ovarian cystectomy)
This procedure is necessary for treating ovarian endometrioma or chocolate cyst. It is crucial for the surgeon to completely remove the entire cyst wall without damaging the normal ovarian structure.
4) Excision of adhesions
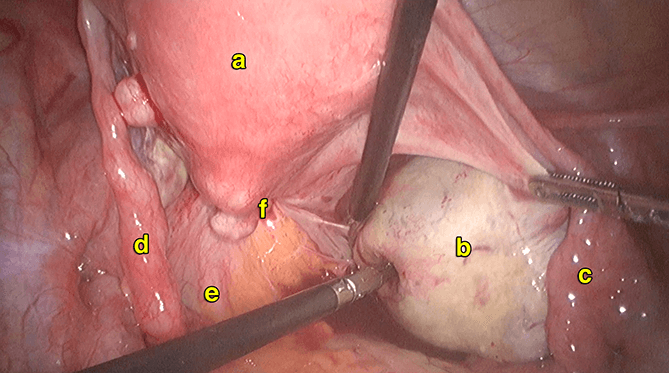
5) Excision of deep infiltrating endometriosis (DIE)
Deep infiltrating endometriosis (DIE) is a specific type of endometriosis in which the endometriotric implants have invaded the wall of the organs. Excision of the implants is
very challenging because only partial excision is necessary. Meticulous skills are required to repair the partially excised organs so that their functionality will not be compromised. Therefore, surgery will not be advised unless the patient is suffering from its symptoms. Specific sites like recto-vaginal septum pose an even higher challenge and risk to the surgery and a multidisciplinary approach involving a bowel surgeon and a urologist is a must.
6) Excision of rectosigmoid and bowel endometriosis

7) Removal of one or both ovaries (oophorectomy)
When the ovary is severely damaged by the ovarian cyst or when the ovarian cyst is too large to be removed via cystectomy, it may be necessary to remove the entire ovary. This is usually considered as a last resort because once both ovaries are removed, hormone production immediately ceases. This will lead to symptoms similar to natural menopause, but in a more intense manner due to the sudden changes in hormone levels.
8) Removal of the uterus (hysterectomy)
This procedure may be necessary in cases of severe endometriosis especially when there is also adenomyosis. It may or may not involve oophorectomy but is typically performed together with excision of endometriotric implants. It is usually considered in women who have completed their family (see Chapter 33).
9) Removal of endometriosis of the bladder

10) Laparoscopic uterosacral nerve ablation (LUNA)
This procedure aims to alleviate chronic pelvic pain by resecting the nerves that link the uterus to the brain.
Recurrence After Surgery
The recurrence rate for endometriosis varies from approximately 10% to 50%. The more severe the endometriosis, the more
likely it will recur. Recurrence occurs particularly because of incomplete or inadequate excision of endometriotic implants. Although it is almost impossible to remove all the endometriotric implants (especially when the disease involves vital structures), it is still important to choose a well-skilled gynaecologist who is able to remove as much of the endometriotic implants as possible during surgery, to lower the recurrence risk.
Preventing Recurrence
In view of the fact that endometriosis is an oestrogen-dependent disease, suppressing oestrogen, may delay or even prevent a recurrence of the disease. One method to do so is to take oral contraceptive pills continuously 3 months at a time (i.e. 4 menstrual cycles per year) in a long-term manner.
Chances of Getting Pregnant
Chances of getting pregnant rely on the severity of the disease. As long as the reproductive function is not interfered with, pregnancy is possible. However, in many cases, endometriosis damages and distorts the anatomy of the reproductive organs, such as causing scarring and blockage in Fallopian tubes as well as, distorting or enlarging the uterus (particularly with adenomyosis). The presence of ovarian endometriomas (chocolate cysts) also damages the ovaries. The damage may become permanent when the cysts grow too large or become twisted. It is therefore important not to delay treatment because the progression of endometriosis may irreversibly narrow the chances of pregnancy.
Choosing A Gynaecologist
Endometriosis surgery is perhaps the most difficult and complex gynaecological operation to perform. It is best performed laparoscopically because of the direct superior visualization of the pelvic cavity. Not only should the surgery be performed in a centre, dedicated to laparoscopy, but also, be performed by a well-trained and experienced laparoscopic surgeon. As endometriosis may involve the bowel, bladder and ureters, the gynaecologist must be able to work with a bowel surgeon as well as a urologist.
Case 25.1
Pregnancy via IVF in a patient who underwent bilateral cystectomy for endometrioma
NHMT came to see me in 2012. She was 27 years of age and had undergone a previous laparotomy and cystectomy for endometrioma at a different hospital in 2010. She was given gonadotrophin releasing hormone agonist for 6 months followed by danazol. She had been married for 2 years and could not conceive. She had also previously done a hysterosalpingogram, which showed a blocked left fallopian tube and a patent right fallopian tube. She complained of slight dysmenorrhea. She had attempted an intrauterine insemination (IUI) in the other hospital, but she was not successful.
Examination and transvaginal ultrasound showed bilateral ovarian cysts measuring 2.14 x 2.51cm (left ovary) and 2.00 x 2.40cm (right ovary). AntiMullerian hormone (a hormone to test the ability of the ovaries to produce oocytes (eggs)) done was in the normal range, indicating that she could still produce oocytes. She was discouraged to undergo another laparoscopic cystectomy and was advised to undergo IVF. She agreed and underwent the procedure in 2012. It was a successful attempt. Only 4 eggs were retrieved and there were only 2 embryos. She conceived and delivered a baby boy in 2013. She is currently on 3 monthly Depoprovera® injections to prevent a recurrence of the endometriosis.
Discussion
This lady underwent a cystectomy for endometrioma. She had a recurrence of the endometriomas but was advised to not undergo a second surgery because of the worry of reducing her ovarian reserve (ability to produce oocytes). She was advised to undergo IVF to increase her chances of pregnancy. The pregnancy itself would cause a reduction in the chances of recurrence and after the delivery she was advised to stop ovulation to reduce the chances of recurrence.
Case 25.2
Spontaneous pregnancy in a young lady who underwent 2 previous laparoscopic cystectomies for large endometriomas
SSMS first me saw at the age of 19 in 2001. She complained of left iliac fossa pain for 3 months. Her menses had been regular but she had been having dysmenorrhea of increasing severity. Examination and abdominal ultrasound showed a large endometrioma of size 4.65 x 4.98 and 4.11 and 3.21cm in diameter. She underwent a laparoscopic cystectomy. She had 2 large endometrioma in her left ovary. The right ovary was normal and both her fallopian tubes were normal. Postoperatively, she was given gonadotrophin realeasing hormone (GnRH) agonist monthly for 6 months. She was well after that. However she returned in 2002 again complaining of increasing dysmenorrhea. Examination and ultrasound done showed bilateral endometrioma of size 3.42 x 3.52cm and 1.75 and 2.25 cm. She underwent a second laparoscopy and was found to have a large right endometrioma and a small left endometrioma. Laparoscopic cystectomy was performed. Postoperatively she received dimetriose for 6 months. She was still single and was advised to take oral contraceptive pills but she refused. She was on regular follow up. She had small ovarian cysts, which were not symptomatic. She got married in 2004 (age 22) and had difficulty in conceiving. Hysterosalpingogram (HSG) done showed a blocked left tube. She was given clomiphene citrate. In 2005 she had another endometrioma in the right ovary measuring 3.06 x 5.04 cm. Surgery was not advised and she was advised to conceive. She conceived spontaneously in 2006 (age 24) and delivered a baby girl by Caesarean section for fetal distress in 2007. She was on oral contraceptives after the delivery till 2010. Again she had difficultly in conceiving. There were no more ovarian cysts seen on ultrasound. She was again prescribed clomiphene citrate. She conceived spontaneously in 2012 (age 30) and delivered a baby
boy in 2013. She is currently well and is on oral contraceptive pills.
Discussion
This young lady developed endometrioma and underwent 2 laparoscopies. Fortunately she got married early and because of her young age managed to conceive spontaneously twice. Preventing recurrence of endometriosis in unmarried women is important. The cheapest way of doing this is by taking oral contraceptives. She refused to take the OCPs when she was single and only took the pills after her first delivery. It is important to note that multiple surgeries on the ovaries can lead to a reduction in the ovarian reserve.


Summary
Laparoscopy is the gold standard for the diagnosis and treatment of endometriosis. The types of operations that can be performed include coagulation, excision of the endometriotic implants, excision of the endometriotic cyst wall (ovarian cystectomy), excision of adhesions, excision of deep infiltrating endometriosis (DIE), excision
of rectosigmoid and bowel endometriosis, removal of one or both ovaries (oophorectomy), removal of the uterus (hysterectomy), removal of endometriosis of the bladder and laparoscopic uterosacral nerve ablation (LUNA). Endometriosis surgery can be complex and should be performed by an experienced laparoscopic gynecological surgeon, assisted by a bowel surgeon and an urologist.
