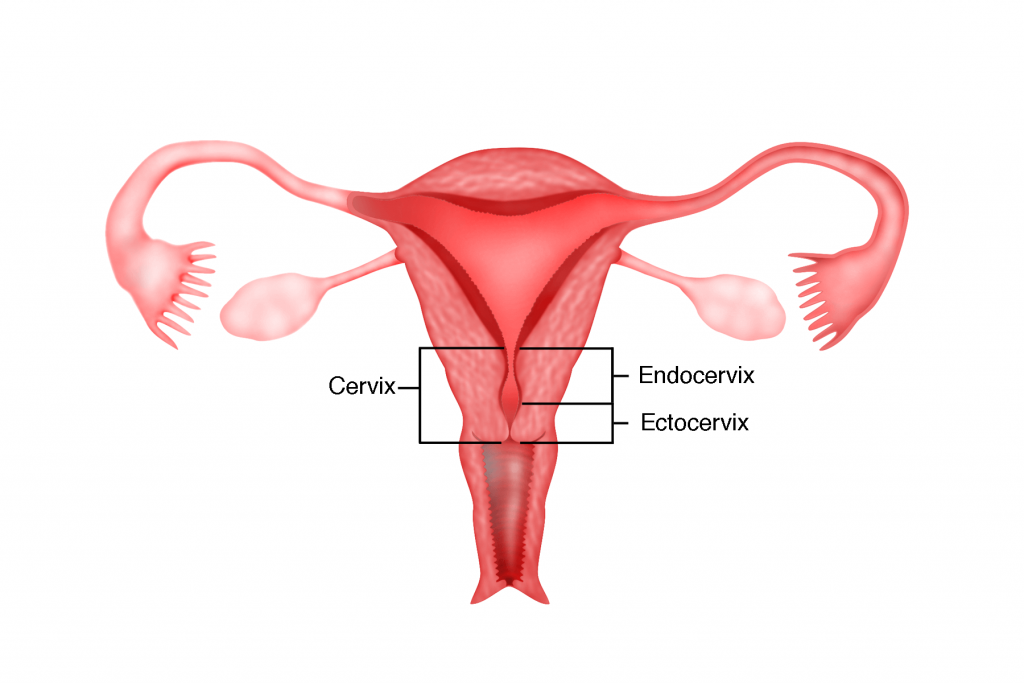
The cervix is the lower constricted segment of the uterus that joins the upper part of the vagina. It consists of 2 parts. The part of the cervix that extends into the vagina is called the ectocervix or porto vaginalis. It is about 3 cm long and 2.5 cm wide. It is lined by flat, fish scale-like cells called the squamous cells. The part of the cervix that is above the vagina is called the endocervix. The endocervix is lined by box-like glandular cells called the columnar cells. The junction between these 2 types of cells is called the transformation zone. This is the part of the cervix that is prone to develop cancer of the cervix.
Types of cancer of the cervix
There are many types of cancer of the cervix but the 2 most common types are:
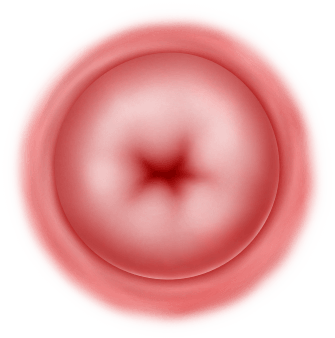
1. Squamous Cell Cervical Cancer
which arises from the squamous cells of the ectocervix
2: Adenocarinoma of the Cervix
which arises from the glandular cells of the endocervix.
Incidence
Due to successful implementation of cervical screening programmes (Pap smear), the incidence of cancer of the cervix is declining worldwide. However, the rate is still high in developing countries. The peak age is 45 – 60 years and its incidence decline after that but peaks again at 80 years of age.
Cause
Cancer of the cervix is thought to be caused by the Human Papilloma Virus (HPV). HPV is a sexually transmitted virus. There are over 100 different types of HPVs – 15 types of these can cause cancer of the cervix in 99% of cases. Approximately, HPV 16 and 18 cause 70% of cases of cancer of the cervix.
Risk Factors
Women with multiple sexual partners have a higher risk.
Becoming sexually active early
Smoking
Weakened immune system
Women with more children (multiparous) have a higher chance of developing cancer of the cervix than women who have never had children
Long term use of contraceptive pills increases the risk slightly.
Women of lower socioeconomic status have a higher risk of cervical cancer compared to women of upper socio-economic status.
Women who are married to men with multiple sexual partners have a higher risk of cervical cancer
Women who are infected with other sexually transmitted diseases such as chlamydia, gonorrhoea or syphilis have a higher risk of developing cervical cancer.
Symptoms
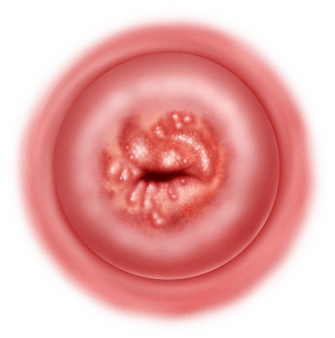
Vaginal bleeding after sexual intercourse
Abnormal watery or blood stained vaginal discharge
Bleeding between periods
Bleeding in post-menopausal women
Pelvic pain
Smelly vaginal discharge
Some patients may not have any symptoms at all and yet be diagnosed with cancer of the cervix during a routine cervical smear
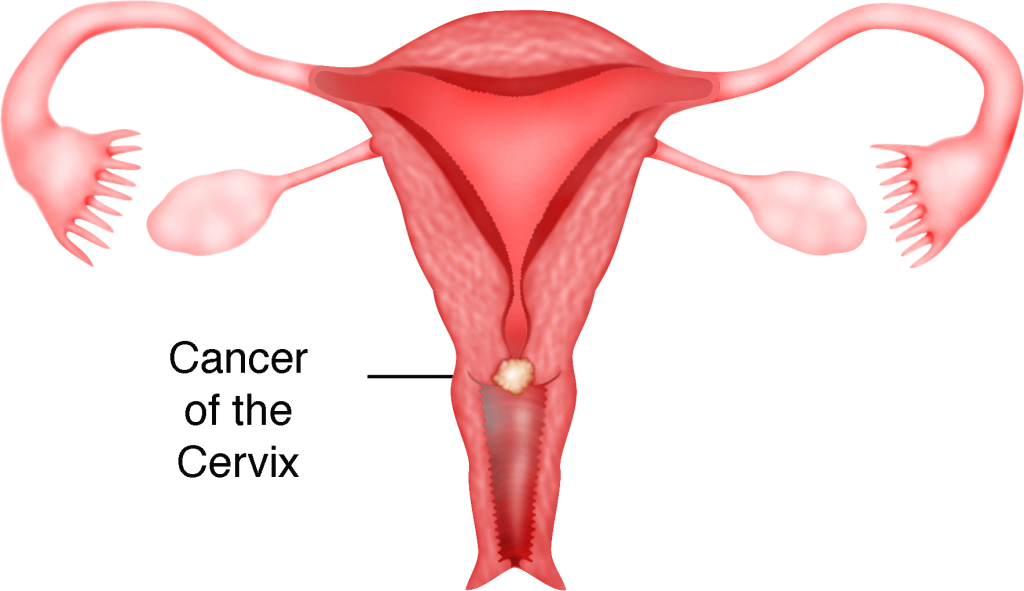
Diagnosis
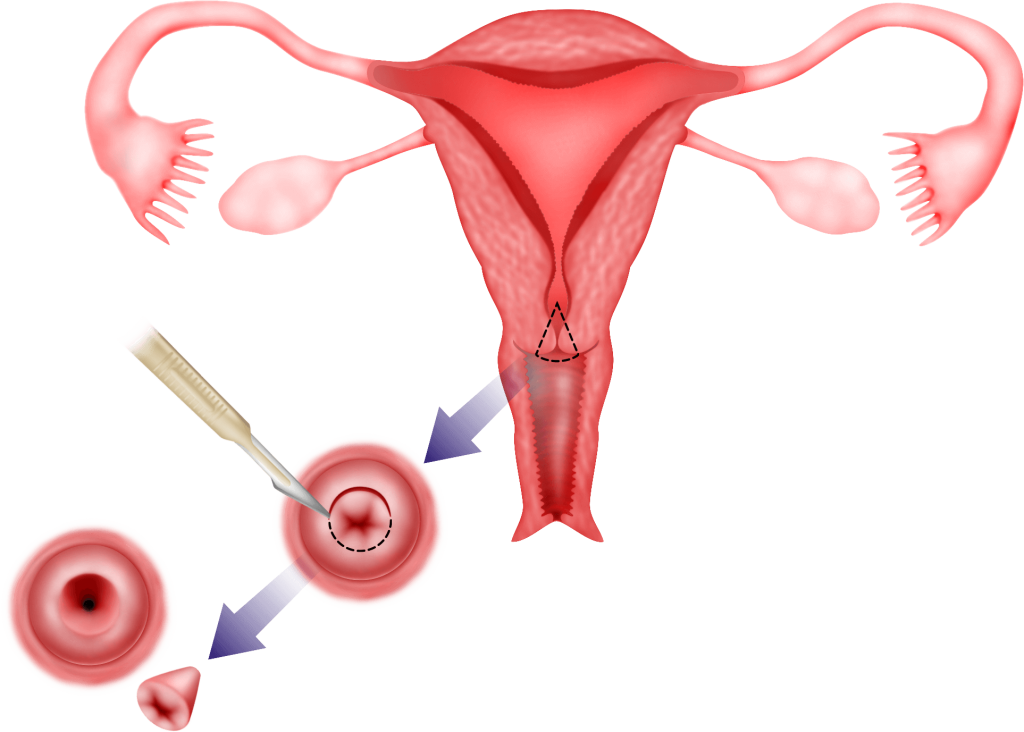
In patients with an obvious cervical lesion, a punch biopsy (g) of the lesion can be done for histopathological (g) examination. If the lesion is not obvious, a colposcopy (g) should be performed and biopsies can be taken. Sometimes a cone biopsy (g) may be necessary to confirm the diagnosis.
Staging of cancer of the cervix
Once the diagnosis of cancer of the cervix has been made, staging of the cancer is necessary. Several tests may be necessary to stage the cancer.
1) Pelvic ultrasound
Transabdominal and transvaginal ultrasound can give an idea of the size of the uterus and ovaries and whether there is any spread of the cancer.
2) CT (computerized tomography) scan or MRI (magnetic resonance imaging) scan
A CT scan or MRI scan can be done to see the size of the tumour and to see the extent of the spread of the tumour
3) Examination under anaesthesia
If a patient is under anaesthesia, the doctor can examine the vagina, cervix and rectum more thoroughly. A cystoscopy can be performed to see whether the cancer has spread to the urinary bladder. A rectal examination and a proctosigmoidoscopy may be performed to see whether the cancer has spread to the rectum.
Stages of cancer of the cervix
Stage 1: The cancer is confined to the cervix
Stage 1A : the cancer can only be visualised through a microscope.
Stage 1A1 : the depth of the cancer is less than 3 mm and the width is less than 7 mm
Stage 1A2 : the depth is between 3- 5mm and the width is less than 7 mm wide
Stage 1B : the cancer is larger and can be visualised by the naked eye but is confined to the cervical tissue and has not spread
Stage 1B1 : the cancer is no larger than 4 cm : the cancer is larger than 4cm
Stage 1B2 : the cancer is larger than 4cm
Stage 2: The cancer has spread to the top of vagina or has reached the tissue around the cervix (parametrium).
Stage 2A : the cancer has reached the top of the vagina
Stage 2B : the cancer has reached the tissue around the cervix (parametrium)
Stage 3: The cancer has spread to the lower third of the vagina and/or reached the pelvic wall
Stage 3A : The cancer has reached the lower third of the vagina, but not the pelvic wall
Stage 3B : The cancer has grown through the pelvic wall
Stage 4: The cancer has spread to the bladder or rectum or has spread further (lungs, liver and bones)
Stage 4A : The cancer has reached the bladder or rectum (nearby organs)
Stage 4B : The cancer has spread further, possibly the lungs, liver or bones
Treatment
Treatment will depend on the stage of the cancer and the health of the patient. Treatment includes surgery, radiotherapy, chemotherapy, combinations of radiotherapy and chemotherapy called chemoradiation or other combination therapies.
1) Surgery
Early cancer of the cervix can be treated by surgery.
Stage 1A1 cancer of the cervix can be treated by just a cone biopsy (g), simple hysterectomy or total laparoscopic hysterectomy (see chapter 33). Cone biopsy is a procedure whereby a cone shaped incision is made around the cancerous tissue and removed.
Stage 1B to 2A cancer of the cervix will require a radical hysterectomy and pelvic lymphadenectomy. These can be performed either by laparotomy or laparoscopy (see chapter 35). After the surgery, if on histopathological examination, it is found that the cancer has spread, additional chemotherapy and/or radiation may be necessary.
2) Chemotherapy and Radiotherapy
In patients with more advanced disease (stage 2B to stage 4), it is not possible to remove all the cancer by surgery. In these patients and in women who are not medically fit to undergo surgery, the usual mode of treatment is a combination of chemotherapy and radiotherapy.
Survival Rates
The 5-year survival rates for cancer of the cervix following appropriate treatment are
Stage | 5 year survival rate |
|---|---|
1 | 81.6% |
2 | 61.3% |
3 | 36.7% |
4 | 12.1% |
Prevention
In 70% of cases, HPV 16 and 18 cause cervical cancer. The HPV vaccine aims to reduce HPV infections in women.
Regular cervical screening (Pap smear) aims to pick up precancerous lesions early. Treatment of these precancerous lesions can prevent progression to cancer.
Summary
Cancer of the cervix is a preventable disease. It is thought to be caused by a virus called the Human Papilloma Virus. Early cervical cancer can be treated by surgery. In more advanced cases, however surgery is not possible and the patient will be treated with radiotherapy and chemotherapy.
